NEURORADIOLOGIA DE EMERGENCIA

Sign up for access to the world's latest research
Abstract
AI
AI
This text discusses the role of neuroradiology in emergency situations, particularly focusing on cerebrovascular emergencies like stroke. It emphasizes the importance of timely imaging to differentiate between ischaemic and haemorrhagic events. The chapter highlights the necessity for neuroradiologists to provide comprehensive morphological and functional information to aid in acute clinical decision-making, especially with the advent of fibrinolytic treatments that enhance the potential for effective interventions.













































































































































![Fig. 2.14 - Bilateral subdural haematomas. There is a biloculat- ed acute-subacute subdural haematoma on the right side (a), a heterogeneous appearance of the two haematomas with fluid- fluid levels (b), and presence of haemorrhagic components of different ages. The left sided subacute subdural haematoma is almost isodense as compared to the underlying brain and is therefore somewhat difficult to visualise. [a), b) axial CT].](https://figures.academia-assets.com/35610716/figure_152.jpg)
![Fig. 2.13 - Axial CT demonstrates an acute subdural haematoma along the left hemisphere convexity with right shift of the mid- line structures and compression of the left lateral ventricle. [a), b) axial CT].](https://figures.academia-assets.com/35610716/figure_153.jpg)

![Fig. 2.16 - Subdural haematoma. Axial CT reveals and unusual appearing left frontoparietal subdural haematoma with a hy- perdense acute haemorrhagic component layering posteriorly. The left lateral ventricle is compressed by the haematoma and the contralateral lateral ventricle is dilated. [a), b) axial CT].](https://figures.academia-assets.com/35610716/figure_155.jpg)
![convex lateral margin; however, in the presence of an SDH this margin becomes flattened, con- cave or irregularly distorted. If the cortico- medullary junction is not visible, a bolus injection of contrast medium administered during the scan may be useful in identifying the cortical surface and delineating the border of an isodense SDH. This image enhancement method can document Fig. 2.18 - Subdural haematomas. Axial and coronal CT shows small, chronic subdural haematoma over the convexity of the brain is observed which is better seen on coronal scans. [a) ax- ial CT; b) coronal CT].](https://figures.academia-assets.com/35610716/figure_156.jpg)
![Fig. 2.17 - Bilateral subdural haematomas. Axial CT shows bi- lateral hypodense subdural haematomas. [a), b) axial CT].](https://figures.academia-assets.com/35610716/figure_157.jpg)


![Fig. 2.21 - Subarachnoid haemorrhage. Hyperdensity is noted within the cortical sulci over the left cerebral hemisphere. Small haemorrhagic cortical contusions are also seen, the largest of which can be observed in the right temporal region (arrow- head). [a), b) axial CT]. SDH’s do not cross the midline because the subdural spaces on the two sides of the crani- um do not communicate. These haematomas are occasionally observed beneath the tempo- ral lobe within the middle cranial fossa and un- der the occipital lobes extending along the ten- torium cerebelli, and are often difficult to see with axial slices alone. In these instances, sup- plemental coronal slices are helpful for visuali- zation.](https://figures.academia-assets.com/35610716/figure_160.jpg)
![Fig. 2.22 - Posttraumatic intraventricular haemorrhage, pneumocephalus, and cerebral oedema. Bilateral eyelid haematomas are seet associated with subcutaneous emphysema (a). Intracranially are observed subarachnoid (b) and intraventricular haemorrhage (a), ai bubbles in the CSF spaces (c) and the widespread oedema within the right cerebral hemisphere (d). [a)-d) axial CT].](https://figures.academia-assets.com/35610716/figure_161.jpg)

![Fig. 2.24 - Posttraumatic cerebral swelling. The CT demon- strated diffuse posttraumatic cerebral swelling is seen with obliteration of the basal subarachnoid cisterns and superficial cortical sulci, compression of the 3" ventricle and reduction in size of the lateral ventricles. The midline structures are not shifted, and there are no focal haemorrhages are present. [a), b), c) axial CT].](https://figures.academia-assets.com/35610716/figure_163.jpg)




![Fig. 2.26 (cont.) - An MRI examination conducted three days later shows an area of hyperintense signal on T1-weighted se- quences (e) and hypointense signal on T2-weighted sequences as a result of haemoglobin breakdown products (i.e., deoxy- haemoglobin). [a), b), ¢) axial CT; d), f) axial T2-weighted MRI; e) axial T1-weighted MRI].](https://figures.academia-assets.com/35610716/figure_168.jpg)
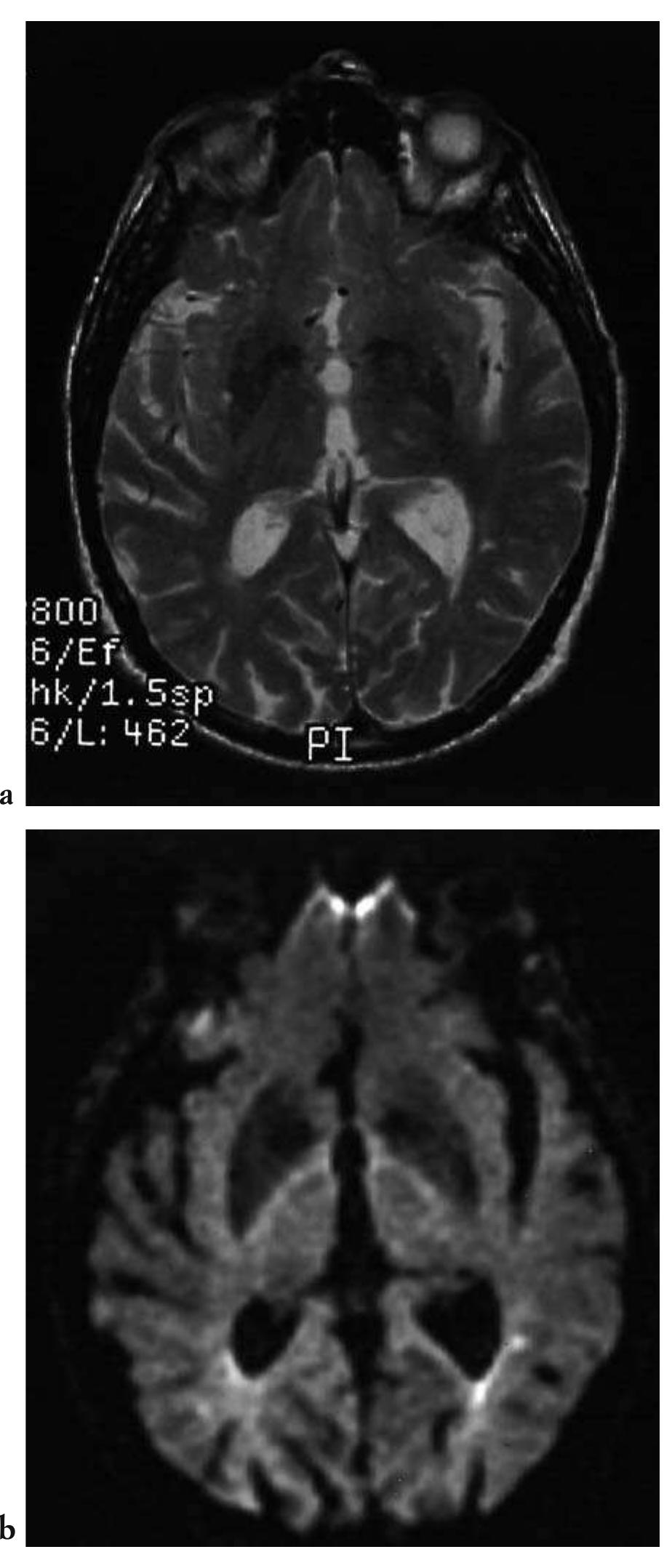
![Fig. 2.27 - Multiple contusive and lacerative haemorrhagic cere- bral foci in the acute phase. The T2-weighted sequence (a) shows multiple areas of signal hyperintensity within which haemor- rhagic components cannot be distinguished. The long scan time often results in motion artefacts. The echo-planar sequence (b), which is more sensitive to T2*-weighted tissue, enables the iden- tification of areas of hypointense signal caused by the presence of subacute haemorrhage (deoxyhaemoglobin). Motion artefacts can also be reduced by obtaining the acquisition in approxi- mately 500 msec. [a) T2-weighted MRI; T2*-weighted MRI].](https://figures.academia-assets.com/35610716/figure_169.jpg)
![Fig. 2.28 - Cerebral contusions. T2 fast spin echo (FSE) and FLAIR sequences demonstrate that the latter prove more sensitive in identifying contusive foci, even of very small dimensions. The superior identification of the subdural haematoma with FLAIR se- quences is also noted. [a), c), d) T2-weighted MRI; b) FLAIR MRI].](https://figures.academia-assets.com/35610716/figure_170.jpg)

![Fig. 2.29 - Hyperacute cerebral haemorrhage. CT and T2- weighted MRI images show that in the hyperacute phase only CT is capable of showing the haemorrhagic component of the right temporal-insular shear-contusive focus. [a) axial CT; b) axial T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_172.jpg)




![Fig. 2.32 - Haemorrhagic shearing injuries. Unlike FSE T2- weighted sequences, gradient recalled echo sequences which are more sensitive to T2* effects, are able to distinguish the presence of a haemorrhagic components within very small grey- white matter junction shearing injuries. [a) T2-weighted MRI, b) T2*-weighted MRI].](https://figures.academia-assets.com/35610716/figure_177.jpg)
























![Fig. 3.2 - Vasogenic oedema caused by malignant cavitary glial neoplasm. The MRI study shows extensive oedema involving the white matter surrounding the neoplasm. Note the mass effect upon the lateral cerebral ventricles and the irregular mural contrast enhance- ment. [a), b) T2-weighted, c) unenhanced T1-weighted, d) and T1-weighted MRI following IV gadolinium (Gd) administration].](https://figures.academia-assets.com/35610716/figure_203.jpg)



![Fig. 3.5 - Mesencephalic tuberculoma with obstructive hydro- cephalus. The MRI shows a contrast enhancing mass lesion of the posterolateral midbrain resulting in stenosis of the aque- duct of Sylvius and obstructive hydrocephalus. [a) axial T2- weighted and b) sagittal T2-weighted MRI; c) coronal T1- weighted MRI following IV Gd].](https://figures.academia-assets.com/35610716/figure_207.jpg)

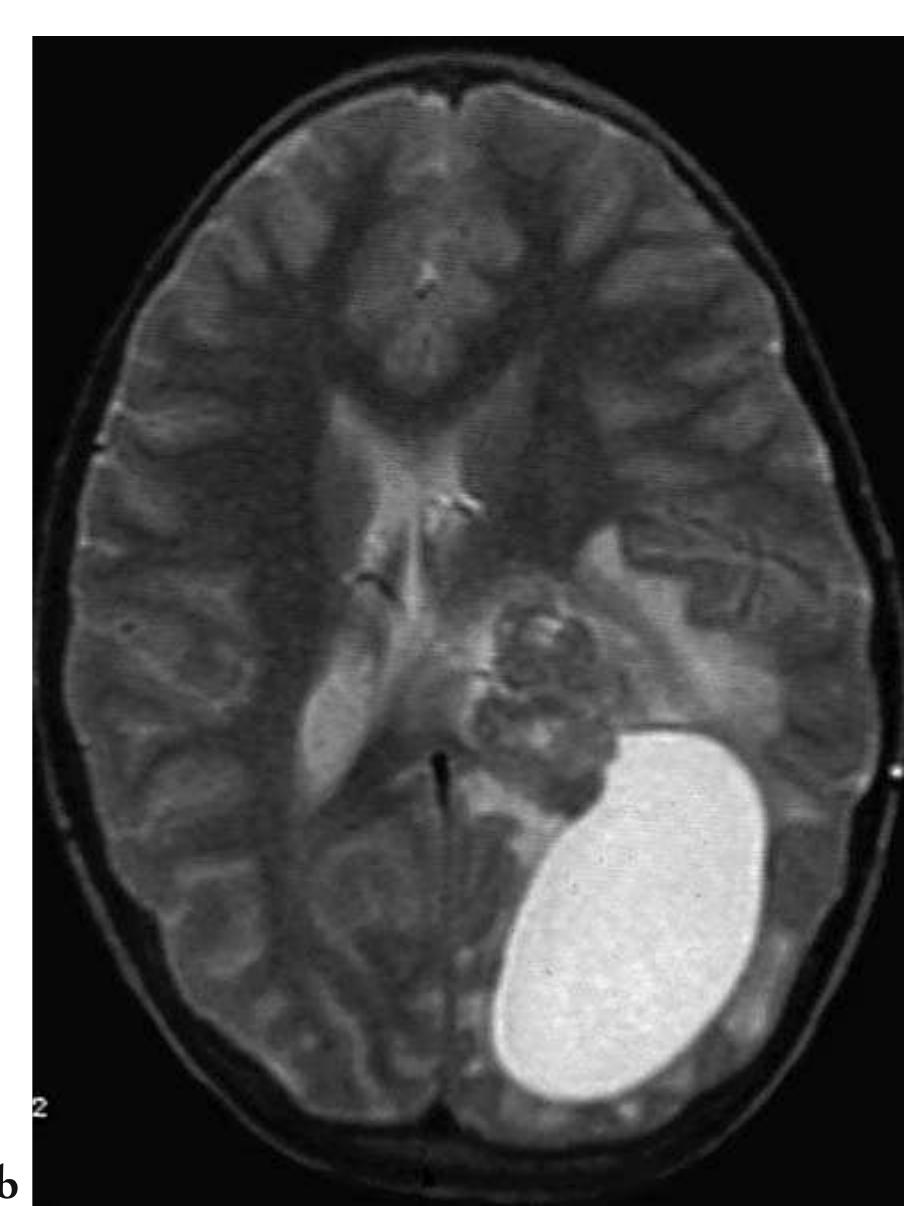
![Fig. 3.6 - Type II Arnold Chiari malformation with obstructive hydrocephalus The MRI examination demonstrates cerebellar tonsillar ectopia, fourth ventricular outlet obstruction and hy- drocephalus. In addition, there is right occipital encephaloma- lacic porencephalic cyst and cervicothoracic syringohydromyelia. [a) sagittal T1- weighted cranial MRI; b) sagittal T1-weighted cervical MRI; c) axial T2-weighted cranial MRI]. After a certain time, chronic inadequate flu- id reabsorption can produce an enlargement of the ventricles without an attendant increase in fluid pressure (normotensive hydrocephalus). In acute hydrocephalus, the CSF is reabsorbed vicariously by the minor resorption systems, firstly by the transependymal pathway, with the appearance of typical findings of hypodensity on CT and hyperintensity on T2-weighted MRI in the periventricular white matter (Fig. 3.8). This absorption pathway is more permeable than the normal one and permits the passage through the periventricular white matter of even large protein molecules.](https://figures.academia-assets.com/35610716/figure_209.jpg)



![Fig. 3.8 - Normotensive communicating hydrocephalus. The MRI images show a thin margin of hyperintensity representing chronic gliosis surrounding the lateral ventricles in a patient with clinically diagnosed chronic normotensive communicating hydrocephalus, not transependymal extravasation of CSF. [a, b) proton density-weighted MRI; c, d) T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_213.jpg)




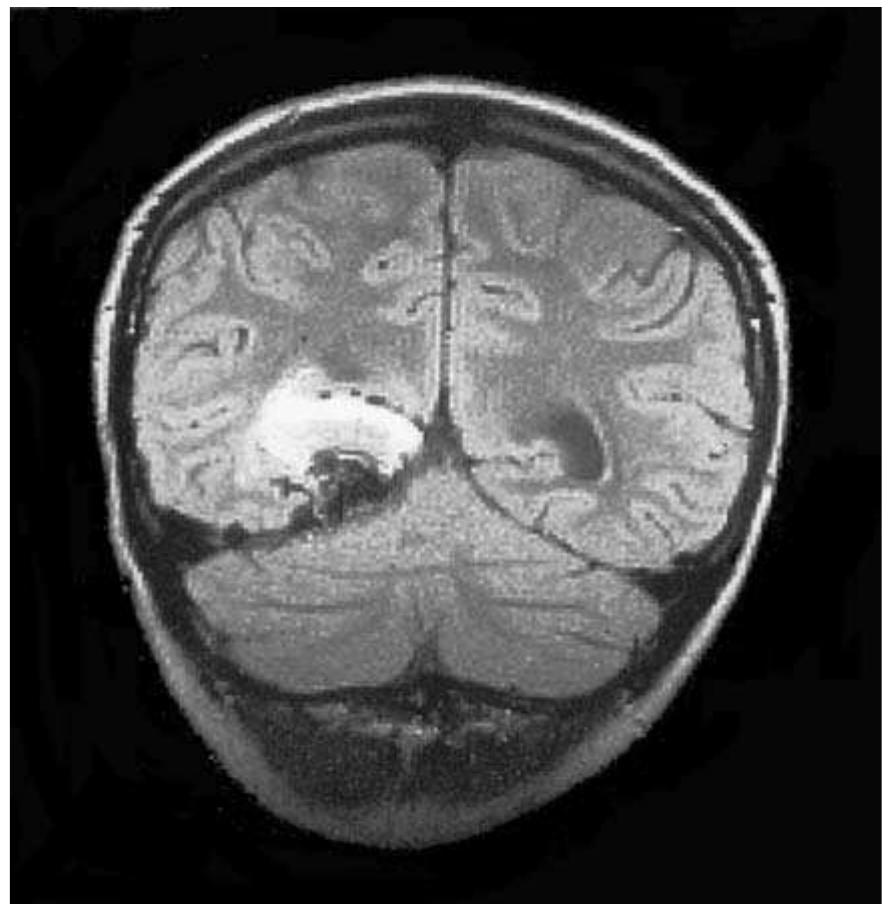
![Fig. 3.11 - Glioblastoma multiforme. The CT and MRI studies show a large, necrotic left hemispheric glioblastoma associated with extensive perilesional vasogenic oedema resulting mass effect and lateral subfalcian herniation. [a, b) unenhanced axial CT; ¢, d, b) PD-, FLAIR, T2-weighted MRI; f, g) T1-weighted axial and coronal MRI following IV Gd].](https://figures.academia-assets.com/35610716/figure_218.jpg)









![Fig. 3.12 (cont.) - h, i) axial and coronal T1-weighted MRI following IV Gd].](https://figures.academia-assets.com/35610716/figure_228.jpg)







![Fig. 3.15 - Postsurgical infection of surgical site. The surgical cavity demonstrates air with irregular contrast enhancement along the resection margins; hypodensity persists in the adjacent white matter due to persistent vasogenic oedema. The CT findings described are of uncertain significance, as they are still compatible with expected postsurgical alterations, however the associated clinical find- ings (headache and high fever) suggest a probable infection of the surgical site. [a, b) unenhanced axial CT; c, d) axial CT following TV contrast].](https://figures.academia-assets.com/35610716/figure_237.jpg)


![Fig. 3.16 - Postsurgical cerebritis. The CT examination shows diffuse hypodensity of the subcortical and deep white matter of the right cerebral hemisphere consistent with oedema, with inhomogeneous contrast enhancement and marked mass effect. The mass re- sults in compression of the ipsilateral ventricle, subfalcian herniation of the midline supratentorial structures and early dilation of the contralateral ventricle caused by obstruction at the level of the foramen of Monro on the left side. The ipsilateral perimesencephalic cistern is obliterated due to downward internal herniation of the uncus of the temporal lobe. [a, b) unenhanced axial CT; c, d) axial CT after IV contrast].](https://figures.academia-assets.com/35610716/figure_240.jpg)




![, Fig. 3.17 - Meningioma of the left pterion. The imaging studies reveal a left frontoparietal homogenously enhancing, broad dural based mass with perilesional oedema and neovascularity originating from the left middle meningeal artery. [a) unen- hanced CT; b, c) left external carotid, left middle meningeal ar- teriogram].](https://figures.academia-assets.com/35610716/figure_245.jpg)
![Fig. 3.18 - Invasive left frontal region meningioma. The skull x-ray demonstrates a large osteolytic lesion of the left frontal region. The CT shows a hyperdense lesion invading the overlying skull and extracranial soft tissues. The angiogram of the left external carotid ar- tery reveals prominent neovascularity originating from branches of the left superficial temporal and middle meningeal arteries. [a) frontal radiograph; b), ¢) axial CT imaged with bone and soft tissue windows; d) left external carotid arteriogram].](https://figures.academia-assets.com/35610716/figure_246.jpg)

![Fig. 3.19 - Olfactory groove meningioma. The right internal carotid arteriogram demonstrates neovascularity associated with a persistent parenchymal blush within a lesion in the ante- rior aspect of the skull base on the right side originating prin- cipally from ethmoid arterial branches. In addition, the right ophthalmic artery in hypertrophied as a result of the increased flow in transit to the neoplasm. [a) frontal projection right in- ternal carotid arteriogram; b) lateral projection right internal carotid arteriogram].](https://figures.academia-assets.com/35610716/figure_248.jpg)


![Fig. 3.22 - Right parietal lobe astrocytoma. Contrast enhanced CT shows mural enhancement within a right parietal lobe sub- cortical mass lesion surrounded by much perilesional oedema. The angiogram of the right internal carotid artery demonstrates no hypervascularity. [a) axial CT following IV contrast; b) lat- eral projection right internal carotid arteriogram] OTHER CEREBRAL NEOPLASMS](https://figures.academia-assets.com/35610716/figure_251.jpg)


![Fig. 3.24 - Right temporoparietal parenchymal metastatic neo- plastic disease. Contrast enhanced coronal CT demonstrates an enhancing mass lesion adjacent to the skull on the right side. The right internal carotid arteriogram in the lateral projection reveals an intensely hypervascular cortical lesion associated with a tumor blush and arteriovenous shunting. [a) coronal CT following IV contrast; b, c) lateral projection right internal carotid arteriogram].](https://figures.academia-assets.com/35610716/figure_254.jpg)
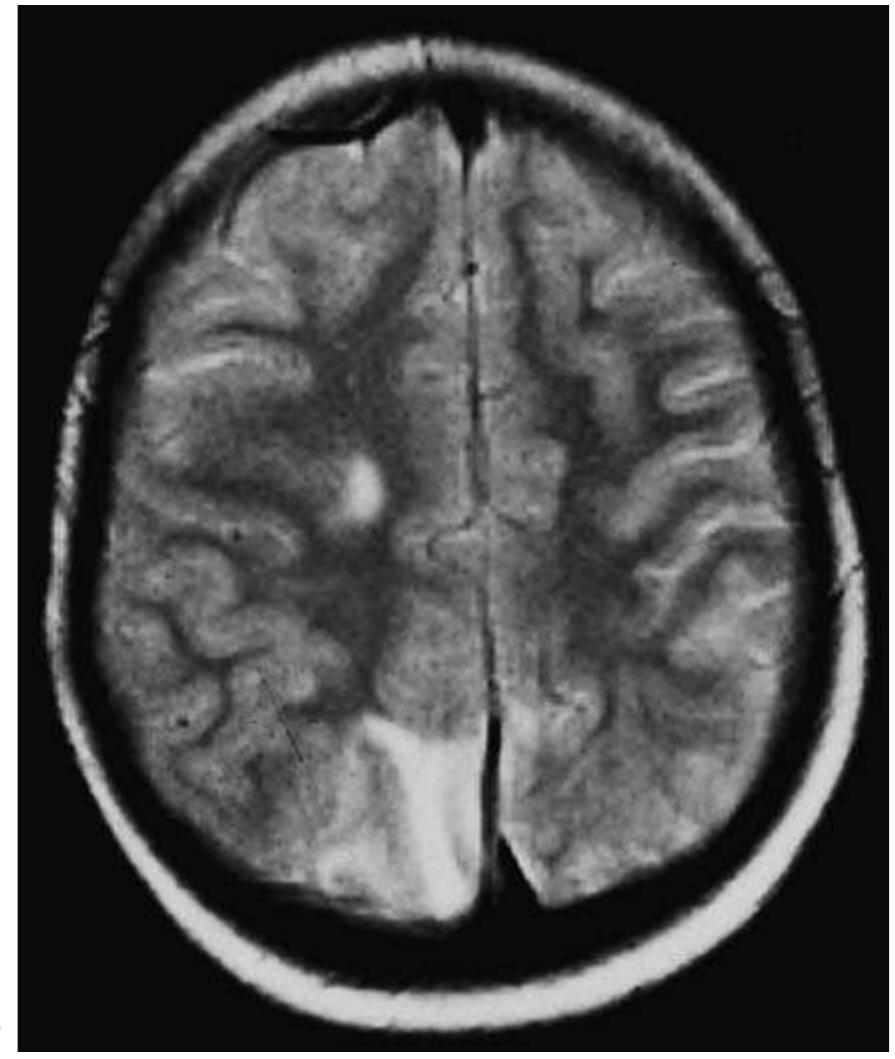
![Fig. 4.1 - Extrapontine myelinolysis in an alcoholic patient. The MRI demonstrates multiple areas of hyperintensity within the hemispheric subcortical hemispheric white matter, the deep hemispheric white matter and the midbrain. [a) coronal FLAIR MRI; b, c, d) axial T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_255.jpg)

![Fig. 4.2 - Two cases of pontine myelinolysis in alcoholic pa- tients. T2-weighted MRI shows a single hyperintense lesion of the pons in each case. [a, b) axial T2-weighted MRI]. The involvement of the mamillary bodies has been demonstrated in 98% of autopsies per- formed on Wernicke sufferers. Using MRI it is possible to demonstrate the involvement of the mamillary bodies primarily in acute cases in which contrast enhancement of the mamillary bodies is observed. However, this finding is not constant and is probably only present in cases in which there is endothelial necrosis with atten-](https://figures.academia-assets.com/35610716/figure_257.jpg)

![Fig. 4.4 - Wernicke’s encephalopathy in an alcoholic patient. Enhanced MRI shows contrast enhancement within the mamil- lary bodies bilaterally. More craniad T2-weighted scans shows abnormal hyperintensity within the posteromedial aspect of the thalami bilaterally and the hypothalamus. [a), b) T1-weighted MRI following IV Gd; c-e) PD- and T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_259.jpg)



![Fig. 4.8 - Hepatocerebral degeneration in patient with cirrho- sis. The MRI demonstrates an abnormal area of high MRI sig- nal intensity in the globus pallidus bilaterally. [a) axial, b) sagit- tal T1-weighted MRI]. There are a number of sources of methanol, which can be present in solvents, industrial liq- uids, perfumes and counterfeit spirits, thus making methanol intoxication relatively com- mon amongst alcoholics. It manifests clinically as general malaise and headache and may progress to stupor and coma. Necrotic areas are visible in the putamen as hypodense on CT scans and as high signal intensity on T2-de- pendent sequences in MR studies (Fig. 4.9). The appearance of these areas can also be af- fected by the presence of haemorrhagic infarc- tion. Other related necrotic areas can be identi- fied in the subcortical white matter and in the frontal cortex (12, 28, 29).](https://figures.academia-assets.com/35610716/figure_263.jpg)


![Fig. 4.11 - Delayed post-hypoxic leukoencephalopathy,. MRI examination performed approximately three hours following admission shows widespread MRI signal hyperintensity of the white matter of the centrum semiovale. Follow up MRI approximately 1 month later shows necrosis within the abnormal hemispheric white matter foci identified on earlier scans. This evolution is consistent with delayed post-hypoxic leukoencephalopathy. As in this case, this phenomenon has been described in heroine addicts following expe- riencing acute cardiorespiratory depression. [a), b) axial T-2 weighted MRI on admission; b) axial T1-weighted MRI on admission; c), one month follow up axial T2-weighted MRI, d) one month follow up T1-weighted MRI]. Intoxication from Methotrexate](https://figures.academia-assets.com/35610716/figure_266.jpg)


![Fig. 4.13 - Acute carbon monoxide intoxication with cerebral necrosis. CT undertaken in the acute phase documents bilateral globus pallidus hypodensity and within the anterior frontal white matter on both sides. CT follow up approximately three weeks later reveals bilateral globus pallidus necrosis; MRI performed the same day as confirms globus pallidus necrosis and the frontal subcortical de- generative alteration. [a, b) acute phase axial CT; c) three week follow up CT; d) three week follow up T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_269.jpg)
![Fig. 4.14 - Acute carbon monoxide intoxication with clinicora- diologic resolution. T2-weighted MRI on patient admission shows swelling of the frontal lobe cortex, more prominent on the right side, resulting from cytotoxic oedema. Follow up MRI performed after clinical resolution reveals regression of the frontal swelling. [a, admission T2-weighted MRI; b) follow up T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_270.jpg)
![Fig. 4.15 - Epidural haematoma. The CT examination shows a biconvex blood collection over the right temporoparietal region asso- ciated with marked mass effect. Note the displacement of the surrounding parenchymal structures associated with leftward midline subfalcian herniation and compression of the right lateral ventricle. In the more caudal scan, ipsilateral downward herniation of the uncus is also clearly visible. In addition, there is a fracture in the right temporal bone, with minor fragment displacement. CT follow up three months later documents encephalomalacia of the posterior temporal lobe, perhaps as a result of infarction secondary com- pression-occlusion of the posterior cerebral artery caused by the uncal herniation. [a,,) initial axial unenhanced CT with brain win- dows; b,,) initial axial CT with bone windows; c) three month follow up axial CT].](https://figures.academia-assets.com/35610716/figure_271.jpg)







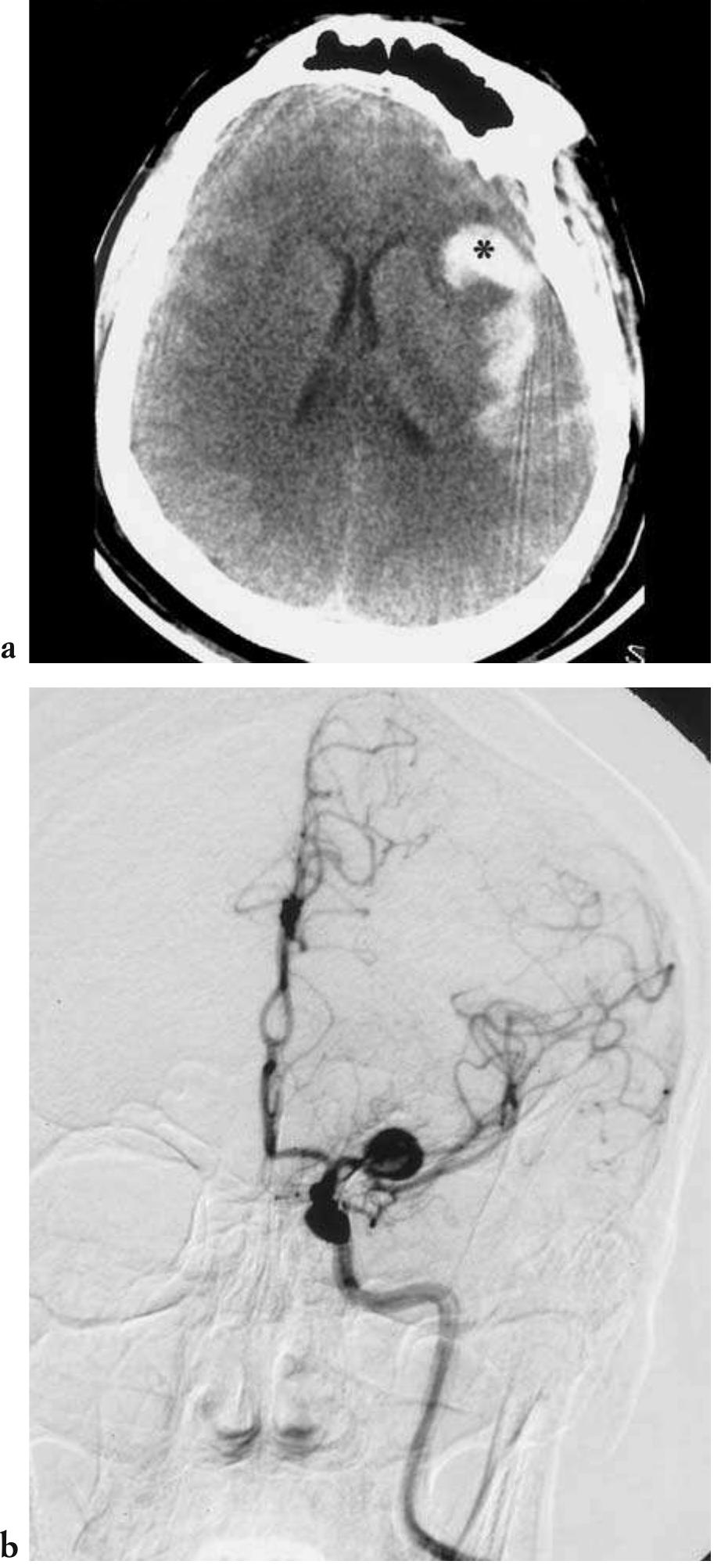
![— CT is the preferred method of imaging in co- ma patients due to its very rapid examination acquisition speeds, with single or multiple slice scanning times faster than one second in latest generation appliances; in addition to its gener- al diagnostic capabilities, it is also very sensitive in recognizing acute and hyperacute phase in- tracranial haemorrhages, in localizing the cra- nial compartment of the bleed (e.g., subdur- al/epidural, subarachnoid, intraparenchymal); finally it is almost universally available in the Fig. 4.17 - Acute hydrocephalus in a case of spontaneous subarachnoid haemorrhage. Unenhanced cranial CT shows an intra- ventricular blood clot at the level of the foramina of Monro and the symmetrical subarachnoid haemorrhage. Also note the di- latation of the lateral ventricles, including the temporal horns, as a consequence of the obstructive hydrocephalus. [a-c) unen- hanced axial CT]](https://figures.academia-assets.com/35610716/figure_279.jpg)



![Fig. 4.19 - Diffuse axonal injury (damage). Unenhanced cranial CT shows the presence of multiple, small cortical-subcortical junction haemorrhagic foci. These haemorrhages are an ex- pression of axonal shearing, some of which are not visible due to the absence of bleeding. The parenchymal, and therefore functional, damage is often greater than predicted on the basis of CT alone. [a, b) unenhanced axial CT].](https://figures.academia-assets.com/35610716/figure_283.jpg)



![Fig. 4.22 - Global hypoperfusion. Unenhanced cranial CT performed 24 hours after a cardiac arrest during heart surgery documents relative isodensity of the lenticular nuclei bilaterally. Axial T2-weighted MRI 48 hours after the event reveals MRI signal hyperinten- sity within the lenticular nuclei. Axial T2-weighted and FLAIR MRI 3 weeks later demonstrates minor dilation of the ventricular sys- tem as a result of resolution of cerebral swelling, and an increase in the hyperintensity of the MRI signal of the lenticular nuclei. The FLAIR image at 3 weeks shows hyperintense cortical-subcortical MRI signal alterations. [a) initial axial CT; b) axial T2-weighted MRI at 48 hours; ¢) axial T2-weighted MRI at 3 weeks; d) axial FLAIR MRI at 3 weeks].](https://figures.academia-assets.com/35610716/figure_287.jpg)




















![Fig. 4.34 - Brain death. SPECT scans reveal a complete absence of cerebral and cerebellar perfusion. [a) axial a), sagittal b) and c) coronal SPECT]. doubts have been voiced concerning the use of conventional cerebral angiography for verifying BD (20).](https://figures.academia-assets.com/35610716/figure_306.jpg)











![Fig. 4.44 - Postoperative intra-axial haemorrhage. Axial CT (a) shows extensive intraparenchymal haematoma in patient recent- ly operated on for large frontal meningioma (b). [a) postopera- tive unenhanced axial CT; b) preoperative T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_318.jpg)





![Fig. 4.51 - Dislocation of surgical appliances following verte- bral collapse in patient with multiple myeloma operated on for posterior stabilisation. [axial CT].](https://figures.academia-assets.com/35610716/figure_324.jpg)














































![Fig. 5.8 - Acute thoracic spine trauma. The MRI images show a burst fracture of the T12 vertebral body, with posterior dis- placement of bony fragments into the central spinal canal and resulting stenosis. There are no visible signal alterations of the spinal cord. [a) Sagittal T1-weighted MRI; b, sagittal T2- weighted MRI; c) axial T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_372.jpg)
![Fig. 5.9 - Acute lumbar spine trauma. The MRI reveals an L2 burst fracture with posterior displacement of the upper portion of the vertebral body into the central spinal canal and conse- quent canal stenosis. [a) sagittal Tl-weighted MRI, b) sagittal T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_373.jpg)



![Fig. 5.11 - Acute cervical spine trauma. MRI in a patient with bilateral C2 pedicle fractures (Hangman fracture). a), b) Sagit- tal, axial T2-weighted MRI. Fig. 5.12 - Acute thoracic spine hyperflexion trauma. The MRI study shows a fracture of the T9-10 vertebrae with anterior wedging of the vertebral bodies. There is also evidence of oede- ma of the involved vertebral bone marrow. The spinal cord, al- though deflected by posterior displacement of the T9 vertebra, does not show intrinsic signs of MRI signal alteration. [a) sagit- tal T1-weighted MRI, b) c) sagittal, axial T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_377.jpg)





![Fig. 5.16 - Acute cervical spine flexion trauma. The MRI ex- amination shows anterior dislocation of C6-C7 associated with marked stenosis of the central spinal canal. The spinal cord is severely compressed at this level, revealing oedema and swelling of the cord above and below the compression. [a) sagittal T1-weighted MRI; b) sagittal T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_383.jpg)
![Fig. 5.17 - Acute cervical spine trauma. The MRI images reveal straightening of the physiologic cervical lordotic sagittal spinal curvature. In addition, there is a compression fracture of the C6 vertebral body. The spinal cord is swollen and is hyperintense on T2*-weighted MRI due to oedema associated with cord con- tusion, but no evidence of acute haemorrhage can be identified. [a) sagittal T1-weighted MRI; b) Sagittal T2*-weighted MRI].](https://figures.academia-assets.com/35610716/figure_384.jpg)

![Fig. 5.18 - Acute cervical spine trauma. The MRI examination shows a loss of the physiologic cervical lordotic sagittal spinal curvature and pre-existent central spinal canal stenosis. A focal area of spinal cord contusion (i.e., oedema and swelling) can be seen on the right side at the C4 level as well as a presumed trau- matic posterior disk herniation associated with underlying spinal cord compression. [a, sagittal T2-weighted MRI; b) axi- al T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_386.jpg)
![Fig. 5.19 - Acute thoracic spine trauma. The MRI acquisitions reveal a compression fracture of the body of T12 associated with T12-L1 anterior subluxation and central spinal canal nar- rowing. In addition, there is a small anterior epidural haematoma at T11. MRI signal hypointensity is present within the spinal cord on the T2* acquisition due to acute haemor- rhagic contusion (deoxyhaemoglobin). a) [sagittal T1-weighted MRI; b) sagittal T2*-weighted MRI].](https://figures.academia-assets.com/35610716/figure_387.jpg)

![Fig. 5.20 - Chronic spinal cord trauma. MRI images in a case of late follow up of a burst fracture of L1 revealing diffuse spinal cord atrophy and a focal area of myelomalacia within the conus medullaris. [a) sagittal T1-weighted MRI; b) sagittal T2- weighted MRI].](https://figures.academia-assets.com/35610716/figure_389.jpg)
![Fig. 5.21 - Chronic spinal cord trauma. MRI in the chronic phase following spinal cord trauma reveals a posttraumatic sy- ringomyelia cavity extending from C6-T1. [a) sagittal T1- weighted MRI; b) sagittal T2-weighted MRI, c) axial T2- weighted MRI].](https://figures.academia-assets.com/35610716/figure_390.jpg)
![Fig. 5.22 - Chronic spinal cord trauma. MRI examination sev- eral years following flexion injury and spinal cord contusion shows postsurgical changes and a multisegmental syringohy- dromyelia cavity of the lower thoracic spinal cord. [a) sagittal Tl-weighted MRI; b sagittal T2-weighted MRI, c) axial T2- weighted MRI]. Fig. 5.21 (cont).](https://figures.academia-assets.com/35610716/figure_391.jpg)










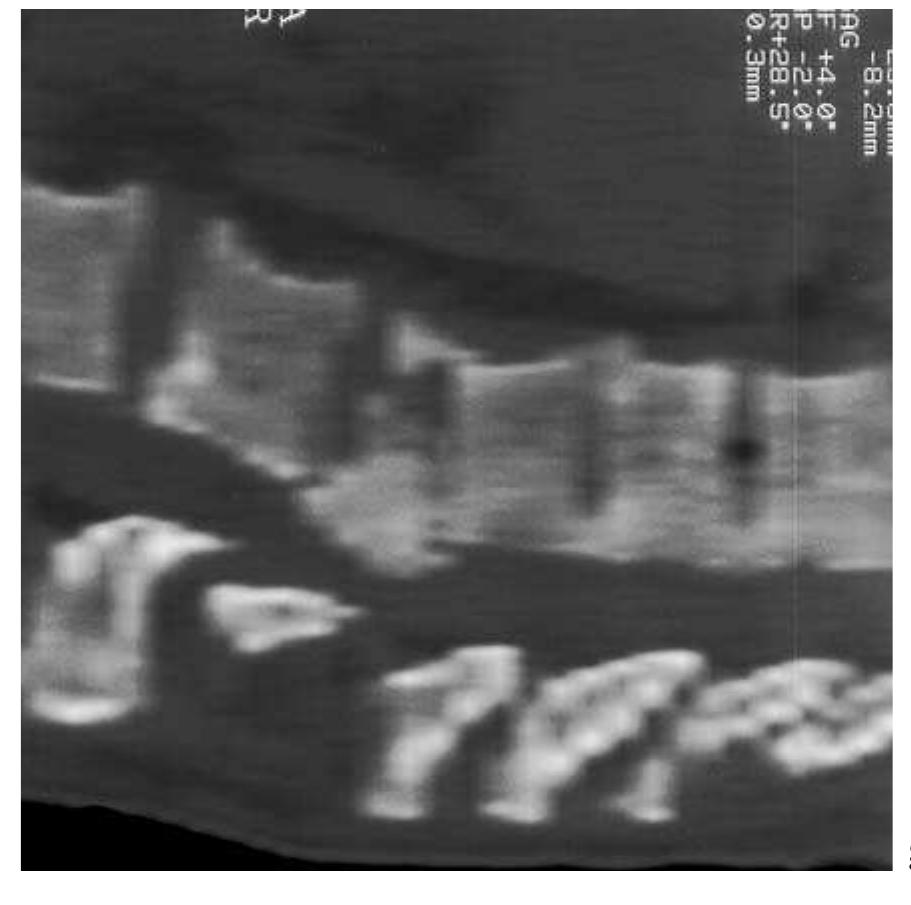
![Fig. 5.26 - Osteoblastoma of the posterior arch of C5. The MRI examination reveals a hypointense lesion within the posterior arch of C5 on the right. The CT study shows a sclerotic mass lesion of the posterior arch of C5. [a) oblique-sagittal T1- weighted MRI; b) axial T1-weighted MRI; c) axial CT].](https://figures.academia-assets.com/35610716/figure_402.jpg)





![Fig. 5.29 - Iatrogenic epidural abscess. The MRI study shows a mass forming posterior epidural lesion that displaces the nerve roots of the cauda equina forwards. There is inhomogeneous enhancement of this process following IV Gd administration. [a) sagittal T2-weighted MRI; b) unenhanced sagittal T1-weighted MRI; ¢) sagittal T1-weighted MRI following IV Gd; d) coronal T1-weighted MRI following IV Gd].](https://figures.academia-assets.com/35610716/figure_408.jpg)




![Fig. 5.31 - Subacute spondylodiskitis caused by brucella species. The MRI study shows a simultaneous pathologic involvement of two adjacent vertebrae and the intervening intervertebral disk. There is irregular contrast enhancement in all involved struc- tures following IV Gd administration. The perivertebral soft tis- sues demonstrate limited involvement. [a) unenhanced sagittal T1-weighted MRI; b) sagittal T1-weighted MRI following IV Gd; c) coronal T1-weighted MRI following IV Gd].](https://figures.academia-assets.com/35610716/figure_413.jpg)


![Fig. 5.33 - Os odontoideum. The MRI images show anterior subluxation of the C1 vertebral body and adjacent odontoid process in relationship to the vertebral body of C2. In addition, the spinal cord is compressed between the posterior bony arch of C1 and the vertebral body of C2, and the intervening spinal cord is hyperintense indicating underlying myelomalacia. Note the partial reduction of the dislocation in extension. [a): neutral T1- and T2-weighted sagittal MRI; b): flexion T1- and T2-weighted sagittal MRI; c): ex- tension T1- and T2-weighted sagittal MRI].](https://figures.academia-assets.com/35610716/figure_416.jpg)
![Fig. 5.34 - Spontaneous subacute epidural haemorrhage in patient with plasmacytopenia. The MRI examination shows mass forming posterior epidural haematoma. IV Gd enhanced MRI shows minor peripheral enhancement around the haematoma. The remaining MRI study reveals hypointensity of the margins of the haematoma consistent with early haemosiderin evolution and anterior spina cord deflection-compression. [a) unenhanced sagittal T1-weighted MRI; b) T1-weighted MRI following IV Gd; c) T2-weighted MRI d) sagittal T2-weighted MRI with fat suppression; e) axial T1-weighted MRI; (f) axial T2-weighted MRI]. The rarer mass-forming lesions of the sub- arachnoid space include (in decreasing order of](https://figures.academia-assets.com/35610716/figure_417.jpg)


![Fig. 5.35 - Extradural arachnoid cysts. The MRI images show a posterolateral intraspinal mass lesion that has an MRI signal that is slightly higher than that of CSF. There is associated cra- nial and caudal displacement of the supra- and subjacent epidural fat surrounding the mass indicating its epidural loca- tion. There is also minor mass effect upon the thecal sac and ex- tension of the cyst into the contiguous, expanded spinal neural foramen. [a) midline sagittal T2-weighted MRI; b) parasagittal T2-weighted MRI; c) midline T1-weighted MRI; d) coronal T1- weighted MRI; e) midlesion axial T2-weighted MRI; f) subja- cent axial T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_420.jpg)




![Fig. 5.37 - Multiple spinal schwannomas in a subject with von Recklinghausen’s disease. The MRI imaging study demonstrates multi- ple intramedullary and intradural-extramedullary masses in the cervicothoracic region, which appear hyperintense on T2-weighted MRI, and show contrast enhancement following IV Gd administration. Also note the multiple perimedullary masses and the numer- ous masses within the nerve roots of the cauda equina. [a) sagittal cervicothoracic T2-weighted MRI; b) sagittal cervicothoracic T1- weighted MRI following IV Gd; c) axial cervical T1-weighted MRI following IV Gd; d) sagittal midthoracic T1-weighted MRI follow- ing IV Gd; e) axial upper thoracic T1-weighted MRI following IV Gd; f): sagittal lumbosacral T1-weighted MRI following IV Gd]. MRI is also useful for the diagnosis of acute spinal cord involvement in multiple sclerosis and sudden onset ischaemic medullary disease. Multiple sclerosis (MS) (6, 9) is a demyelinating disease that most frequently affects females, and which presents with variable neurological](https://figures.academia-assets.com/35610716/figure_426.jpg)



![Fig. 5.38 - Intradural spinal metastasis in a patient with primary intracranial pinealoblastoma. The MRI examination shows that the spinal cord is compressed posterolaterally by an enhancing intradural-extramedullary mass consistent with subarachnoid dissemination of the pinealoblastoma. [a) sagittal T2-weighted MRI, b) sagittal T1-weighted MRI; c) axial T1-weighted MRI following IV Gd].](https://figures.academia-assets.com/35610716/figure_430.jpg)




![Fig. 5.42 - Ependymoma of the conus medullaris. The MRI study shows a septated partially cystic mass with a mural nodu- lar area of contrast enhancement. [a) sagittal T2-weighted MRI, b) sagittal T1-weighted MRI following IV Gd].](https://figures.academia-assets.com/35610716/figure_435.jpg)




![Fig. 5.44 - Ischaemia of the thoracic spinal cord associated with spinal dural arteriovenous fistula. T-2 weighted MRI demon- strates high signal intensity within the central region of the conus medullaris associated with central medullary hyperinten- sity and vascular flow voids over the posterior surface of the thoracic spinal cord. [a) sagittal T1-weighted MRI; b) axial T2- weighted MRI; c) axial T-weighted MRI].](https://figures.academia-assets.com/35610716/figure_440.jpg)
![Fig. 5.43 - Thoracic intramedullary multiple sclerosis. T2 weighted MRI shows an area of intramedullary high signal in- tensity at the T8-9 level associated with minor focal swelling of the spinal cord. Contrast enhancement is seen within the area of MRI signal abnormality following IV Gd administration. [a) sagittal T2-weighted MRI; a) sagittal T-1 weighted MRI follow- ing IV Gd].](https://figures.academia-assets.com/35610716/figure_441.jpg)

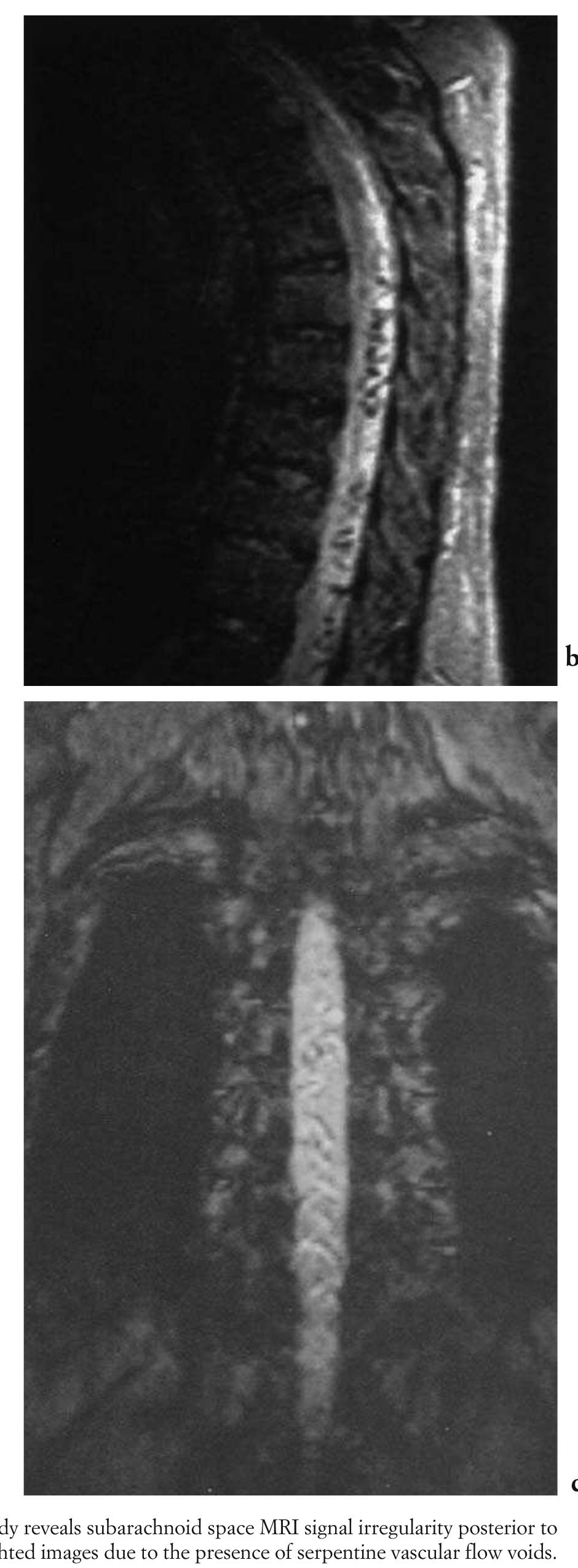

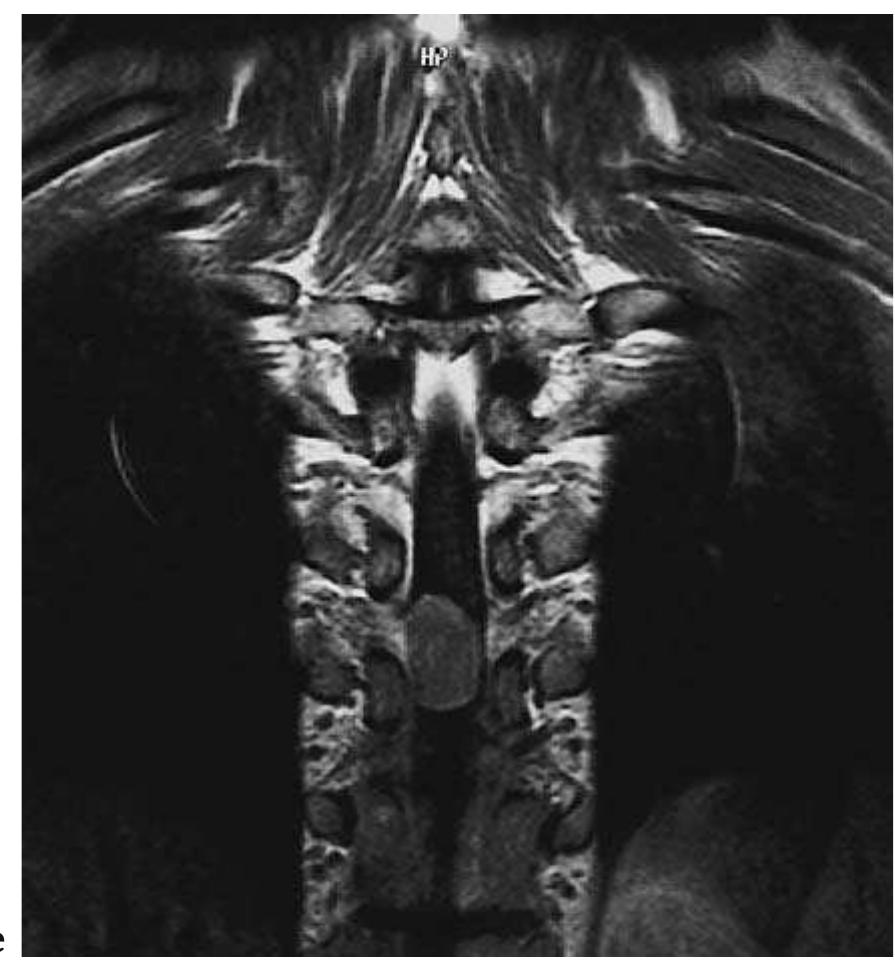
![Fig. 5.45 - Thoracic spinal dural arteriovenous fistula. The MRI study reveals subarachnoid space MRI signal irregularity posterior to the spinal cord, which becomes much more evident on the T2-weighted images due to the presence of serpentine vascular flow voids. [a) sagittal T1-weighted MRI; b) sagittal T2-weighted MRI, c) coronal T2-weighted MRI].](https://figures.academia-assets.com/35610716/figure_445.jpg)






![Fig. 5.48 - Radiation induced thoracic myelitis/spondylitis three years following radiotherapy. T2-weighted MRI with fat suppression shows hyperintense MRI signal within the thoracic spinal cord and within the bone marrow of several contiguous vertebral bodies, both of which are caused in this case by the preceding radiation therapy. Axial T2*-weighted images demonstrate again the intramedullary location of the patholog- ic process. No contrast enhancement of the intramedullary process can be identified. Note the postsurgical alterations. [a) sagittal T2-weighted MRI; b) sagittal T1-weighted MRI follow- ing IV Gd; c) axial T2*-weighted MRI].](https://figures.academia-assets.com/35610716/figure_452.jpg)








































Related papers
2009
This scientific statement is intended for use by physicians and allied health personnel caring for patients with transient ischemic attacks. Formal evidence review included a structured literature search of Medline from 1990 to June 2007 and data synthesis employing evidence tables, meta-analyses, and pooled analysis of individual patient-level data. The review supported endorsement of the following, tissue-based definition of transient ischemic attack (TIA): a transient episode of neurological dysfunction caused by focal brain, spinal cord, or retinal ischemia, without acute infarction. Patients with TIAs are at high risk of early stroke, and their risk may be stratified by clinical scale, vessel imaging, and diffusion magnetic resonance imaging. Diagnostic recommendations include: TIA patients should undergo neuroimaging evaluation within 24 hours of symptom onset, preferably with magnetic resonance imaging, including diffusion sequences; noninvasive imaging of the cervical vessel...
Stroke; a journal of cerebral circulation, 2009
This scientific statement is intended for use by physicians and allied health personnel caring for patients with transient ischemic attacks. Formal evidence review included a structured literature search of Medline from 1990 to June 2007 and data synthesis employing evidence tables, meta-analyses, and pooled analysis of individual patient-level data. The review supported endorsement of the following, tissue-based definition of transient ischemic attack (TIA): a transient episode of neurological dysfunction caused by focal brain, spinal cord, or retinal ischemia, without acute infarction. Patients with TIAs are at high risk of early stroke, and their risk may be stratified by clinical scale, vessel imaging, and diffusion magnetic resonance imaging. Diagnostic recommendations include: TIA patients should undergo neuroimaging evaluation within 24 hours of symptom onset, preferably with magnetic resonance imaging, including diffusion sequences; noninvasive imaging of the cervical vessel...
Clinical Medicine, 2010
Transient ischaemic attack (TIA) is the sudden onset of focal neurological dysfunction of presumed vascular origin that, by definition, resolves within 24 hours (usually much sooner). Its importance as a predictor of completed stroke has only recently been recognised. Updated guidance on the recognition and management of TIA has recently been published as part of the National Clinical Guideline for Stroke. This is a concise version of the TIA component of the full guideline that recommends an urgent response to TIA to prevent subsequent stroke.
Journal of Biomedical and Clinical Research, 2017
SummaryA Transient Ischemic Attack (TIA) is a state of emergency and an independent risk factor for ischemic stroke. The social significance of the disease is determined, based on the probability of occurrence of subsequent cerebrovascular incidents and their frequency among groups. The purpose of the present study was to perform a comparative analysis of clinical features and outcome in patients with TIA for at least 24 months after onset had been registered, according to the pathogenesis and to ABCD (2) score. Two hundred and fifty-seven patients were monitored at the Neurology Clinic, First MHAT – Sofia after suffering an initial TIA. All subjects were studied using a clinical evaluation of pathogenetic mechanisms and an ABCD (2) algorithm. A diagnosis of TIA was confirmed by neuroimaging. The comparison between specific pathogenetic mechanisms demonstrated a statistically significant difference. Two TIA subgroups were involved – thromboembolic and cryptogenic (p<0.05). Also, ...
Geriatric Diseases, 2018
TIA frequency increases with age reaching 10.2% in males and 7.4% in females and decreased in subjects of both sexes aged 85 years or over. The symptoms of TIA vary widely depending on the area of the brain involved. Medical history of specific symptoms and thorough neurological and cardiovascular examinations provide the most important information to diagnose a TIA. TIA poses considerable difficulty in diagnosis, and diagnostic uncertainty is common. Patients presenting with TIA or minor stroke are at high risk of early stroke up to 10% in the first 48 h. Current international guidelines have adopted the ABCD2 score in risk stratification of patients with TIA. For a new-onset TIA patient, an ABCD2 can be a guide in the management.
SiSli Etfal Hastanesi Tip Bulteni / The Medical Bulletin of Sisli Hospital, 2018
The Review of Transient Ischemic Attack Patients: An Experience of a Clinic about Diagnosis and Follow-up T ransient ischemic attack (TIA) is an entity characterized by short-term symptoms of acute, focal cerebral or monocular dysfunction that develops due to insufficient blood flow. Generally, episodes lasting less than 24 hours are considered as TIA. TIA is present in 10-5% of patients with ischemic stroke. [1-4] Eighteen percent of these patients experience a stroke within the first three months and half of them within the first 48 hours. [5] The importance of this condition is that secondary prophylactic therapies to be initiated can prevent stroke. Therefore, the risk of near-term stroke in patients is determined by ABCD2 scoring (age, blood pressure, type of TIA, duration) after TIA, so possible Objectives: Transient Ischemic Attack (TIA) is due to a temporary lack of adequate blood and oxygen to the brain. TIAs typically last less than 24 hours. 10-15% of ischemic stroke patients have a history of TIA. 18% of them experience an ischemic stroke within 90 days, and the ABCD2 scoring system is used to estimate the risk. Our study aims to investigate the risk factors, the etiology, the lesion occurrence on MRI and the near-term risk of stroke of patients on whom TIA was diagnosed. Methods: In this study, 124 patients were included between January 2012 and January 2018. Sixty-eight of the 124 patients were male. The history of patients was questioned; systemic and neurological examinations were made. The stroke risk factors and TIA duration were noted and ABCD2 scores were calculated. All the patients' blood samples, including glucose and lipid profile, were studied. They received CT, DWI MRI, electrocardiography, transthoracic echocardiography, ultrasound and/or MR angiography of the cervical arteries. Results: One hundred twenty-four patients were included in this study, and 56 patients were female. The mean age was 63.04±16.77. Hypertension was the most common risk factor (50.8%). Twenty-seven patients were on antithrombotic; six patients were on anticoagulant therapy, while 91 patients were not receiving any antiaggregan therapy. ABCD2 scores were significantly higher on the antithrombotic therapy group (p=0.019). In 52 patients ABCD2 score was below 4, and in 72 patients, the score was greater than 4. In 67.7% of patients, no etiology was found. An ischemic lesion was detected in 16.9% of the patients. 58 % of the patients were discharged on anticoagulant therapy. Five patients developed ischemic stroke. Conclusion: The risk factors of ischemic stroke and TIAs are similar factors. The etiology of TIAs cannot be found out in most of the patients. Thus, the patients are discharged with oral anticoagulant treatment.
Stroke, 2003
Background and Purpose-Recent studies suggest that the short-term risk of stroke may be greater after transient ischemic attack (TIA) than after stroke. Methods-We compared risks of neurological deterioration in those with and without TIA in the National Institute of Neurological Disorders and Stroke (NINDS) tissue plasminogen activator (tPA) trial, a randomized trial of intravenous tPA given within 3 hours of onset of cerebral ischemia, after excluding those with cerebral hemorrhage and those dying before 90 days of causes other than new ischemic stroke. TIA was defined as a National Institutes of Health Stroke Scale (NIHSS) score of zero at 24 hours. We chose subsequent deterioration as our outcome, defined as a worsening on the NIHSS at 90 days compared with 24 hours, so that episodes of new ischemia that may have been attributed to other causes would be included. Results-Of 498 subjects meeting entry criteria, 40 (8%) had TIA. Subsequent deterioration occurred in 30% of those with TIA and 10% of others (Pϭ0.001, Fisher exact test). In multivariable models with adjustment for age, sex, ethnicity, 24-hour NIHSS score, tPA administration, presumed stroke subtype, and baseline systolic blood pressure, temperature, and glucose, TIA was an independent predictor of subsequent deterioration (odds ratio, 5.0; 95% CI, 2.0 to 12.5; Pϭ0.001). Subsequent deterioration was not associated with tPA treatment, and there was no interaction between tPA administration, TIA, and subsequent deterioration. Lesser degrees of substantial acute recovery were also associated with greater risk of subsequent deterioration.
The New Zealand medical journal, 2013
Transient ischaemic attack (TIA) can be defined as symptoms consistent with stroke that resolve within 24 hours. The public and many health professionals refer to TIAs as 'mini-strokes', terminology that belies their potentially serious prognosis. Although people make a full recovery from a TIA, acute ischaemic lesions revealed on MRI scans occur in just under half of patients.
The Western journal of medicine, 1987
Transient ischemic attack (TIA) is a common but poorly understood disorder. Although it rightfully has been classified as a major risk factor for stroke, the majority of patients with TIAs do not suffer subsequent stroke, and it is unclear whether aggressive evaluation and treatment of TIA will significantly lower stroke risk. To effectively treat this disorder, the implications of transient cerebral ischemia and the basic pathophysiologic process underlying this condition must be understood, as well as the myriad of specific clinical causes that must be considered in any patient. Any less sophisticated approach will only propagate the confusion that already exists and lead to the use of therapies that may be useless or even harmful.
Journal of Neurology, Neurosurgery & Psychiatry, 2005
Expert Review of Cardiovascular Therapy, 2005
American family physician, 2004
Transient ischemic attack is no longer considered a benign event but, rather, a critical harbinger of impending stroke. Failure to quickly recognize and evaluate this warning sign could mean missing an opportunity to prevent permanent disability or death. The 90-day risk of stroke after a transient ischemic attack has been estimated to be approximately 10 percent, with one half of strokes occurring within the first two days of the attack. The 90-day stroke risk is even higher when a transient ischemic attack results from internal carotid artery stenosis. Most patients reporting symptoms of transient ischemic attack should be sent to an emergency department. Patients who arrive at the emergency department within 180 minutes of symptom onset should undergo an expedited history and physical examination, as well as selected laboratory tests, to determine if they are candidates for thrombolytic therapy. Initial testing should include complete blood count with platelet count, prothrombin ...
The New Zealand medical journal, 2009
This review is a summary of the New Zealand guideline for the management of Transient Ischaemic Attack (TIA). TIA is a medical emergency and warrants urgent attention. The risk of early stroke following TIA may be as high as 12% at 7 days, and 20% at 90 days, with half of these strokes occurring within the first 48 hours. All people with suspected TIA should be assessed at initial point of health care contact for their risk of stroke. Diagnosis of TIA is more likely to be correct if the history confirms: sudden onset of symptoms, with maximal neurological deficit at onset; symptoms typical of focal loss of brain function such as unilateral weakness or speech disturbance; and rapid recovery, usually within 30-60 minutes. The ABCD2 score is a tool that assists with diagnosis and identifies people most at risk of stroke after TIA. People at high risk of stroke require urgent specialist assessment as soon as possible but definitely within 24 hours. This includes those with ABCD2 scores ...
European Neurological Review, 2008
More than 700,000 acute strokes 1 and 300,000 transient ischaemic attacks (TIAs) 2,3 occur annually in the US. It is estimated that between 15 and 26% of acute stroke cases have a prior history of TIA. 4 TIAs are important because they are associated with high short-term risk of both stroke and cardiac events. In a widely quoted emergency department (ED) study of over 1,700 TIA cases from California, the three-month stroke risk was found to be 10.5%. 5 A recent meta-analysis of 11 TIA cohort studies found that the summary estimate for the 90-day stroke risk was 9.2%very similar to the Californian study. 6 This meta-analysis also confirmed that most of this stroke risk occurs in the first few days after the TIA event; the risk of stroke was 3.5% at two days and 8.0% at 30 days. 6 Similar findings were found in another recent meta-analysis of 18 cohort studies, which estimated that the seven-day risk of stroke was 5.2%. 7 Patients with TIA are also at high risk of other cardiovascular events. In a meta-analysis of 39 cohort studies, the annual risk of myocardial infarction and non-stroke vascular death following TIA was 2.2 and 2.1%, respectively. 8 These studies, which serve to illustrate the high risk of cardiovascular events following a TIA, suggest that patients suspected of having a TIA event require an expedited clinical work-up.
The American Journal of Emergency Medicine, 2012
Many patients with transient ischemic attacks (TIA) are at high risk of stroke within the first few days of onset of symptoms. Emergency physicians and primary care physicians need to assess these patients quickly and initiate appropriate secondary stroke prevention strategies. Recent refinements in diagnostic imaging have produced valuable insight into risk stratification of patients with TIA. Clinical data regarding urgent initiation of antiplatelet therapy specifically in this patient population with noncardioembolic TIA are limited but promising. This review outlines the diagnostic tools available for rapid assessment of patients presenting with symptoms of TIA and discusses clinical trials that apply to these vulnerable patients.
Journal of the Ceylon College of Physicians, 2020
TIAs predict stroke risk A transient ischaemic attack (TIA) is not a simple 'mini-stroke', but a major warning sign of an impending stroke that demands urgent attention. About 15-30% of all ischaemic strokes are preceded by TIAs 1-4. The estimated recurrent TIA and stroke risk at three months after a TIA is 17.3% 1 ; the risk of stroke is greatest immediately after a TIA, providing only a short window of opportunity for stroke prevention 2. 52% of all strokes during the first 7 days and 42% of all strokes during the first 30 days following a TIA do occur within the first 24 hours 2-5. Early and optimal treatment of TIA has been shown to be effective in prevention of recurrent The changing face of transient ischaemic attacks This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
BMC Neurology, 2015
Background: Patients with transient ischemic attack (TIA) have an increased risk of vascular events. There is scarce data regarding the prognosis of patients with transient neurological symptoms less typical of TIA, in whom a vascular origin cannot be excluded, also known as possible TIA. In this study we aimed to compare the short-term prognosis between TIA and Possible TIA patients. Methods: Patients with transient neurological events consecutively referred to a TIA Clinic during five years were classified as TIA, Possible TIA or mimic. Patients were prospectively followed. We compared the outcome at 30 and 90 days after TIA or Possible TIA. The primary outcome was stroke and the secondary outcome was a combination of vascular events (stroke, TIA, myocardial infarction or vascular death).
Archives of Internal Medicine, 2000
Background: Patients with transient ischemic attack (TIA) or stroke frequently first contact their primary care physician rather than seeking care at a hospital emergency department. The purpose of the present study was to identify a group of patients seen by primary care physicians in an office setting for a first-ever TIA or stroke and characterize their evaluation and management. Methods: Practice audit based on retrospective, structured medical record abstraction from 27 primary care medical practices in 2 geographically separate communities in the eastern United States. Results: Ninety-five patients with a first-ever TIA and 81 with stroke were identified. Seventy-nine percent of those with TIA vs 88% with stroke were evaluated on the day their symptoms occurred (P=.12). Only 6% were admitted to a hospital for evaluation and treatment on the day of the index visit (2% TIA; 10% stroke; P=.03); only an additional 3% were admitted during the subsequent 30 days. Specialists were consulted for 45% of patients. A brain imaging study (computed tomography or magnetic reso

Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
 Frannk Christian Veggro Rios
Frannk Christian Veggro Rios