Isolated Colonic Amyloidosis: An Uncommon Cause of Chronic Diarrhea
American Journal of Gastroenterology

Sign up for access to the world's latest research
Abstract
Results: Out of 4,015 colonoscopic encounters, 352 patients satisfi ed the inclusion criteria for the study. Th ere were 47.1% African Americans, 45.7% Hispanics, 5.5% Caucasians, and 1.7% others. Th e mean age for the cohort was 63.3 years (SD 10.2). Th ere were no signifi cant diff erences in the demographics among the three groups. Group A, B, and C included 210, 94, and 48 patients, respectively. Th e bowel preparation was rated as poor in 46.6% of A, 52.1% of B, and 50% of C (p=0.6). ADR was 24.3% in A, 20.2% in B, and 27.1% in C (p=0.6). AADR was 12.9% in A, 11.7% in B, and 18.8% in C (p=0.4). Th ere was no statistically signifi cant diff erence in ADR and AADR among the groups on accounting for bowel preparation. Conclusion: Th e level of control of diabetes may have no impact on the quality of bowel preparation, adenoma detection rate, and advanced adenoma detection rate. Larger studies are warranted to validate these fi ndings.




![[642] Figure 1: Subsquamous adenocarcinoma under low power. Discussion: To the best of our knowledge, only three definitive cases of subsquamous adenocarci- noma post-RFA have been reported in the literature. One of the patients had a nodule, whereas the other appeared endoscopically normal. Our case had an endoscopically normal-appearing post- ablation esophagus. These emerging reports of subsquamous adenocarcinoma highlight important aspects regarding the endoscopic management of dysplastic BE. First, surveillance biopsies should be performed from the entire length of the original Barrett’s segment despite endoscopically normal-appearing esophageal mucosa. Second, the biopsies should be performed meticulously (Seattle protocol), and ensuring adequate depth to include subepithelial tissue. Finally, utilizing dedicated gastrointestinal pathologists and consensus diagnosis and management plans are abso- lutely imperative.](https://figures.academia-assets.com/72315061/figure_004.jpg)
![Purpose: We describe a minimally invasive treatment option for chronic refractory dysphagia due to presbyesophagus-associated acute angulation of the distal esophagus. The patient is an 80-year- old man who has had chronic post-prandial vomiting and dysphagia for over 10 years. EGD with biopsies, manometry and imaging studies were all normal. Antacids, Savary dilation and Botox therapy yielded only slight improvement. Patient had been on a liquid and pureed diet, but solid foods continued to cause dysphagia with regurgitation. Repeat esophagram revealed a torturous distal esophagus with a 90-degree angulation causing a “zig-zag” appearance where a barium pill had obstructed [FIG 1A]. This angulation was further verified by EGD [FIG 1B]. The patient was not a surgical candidate, so a 22 x 120-mm fully covered SEMS (Boston Scientific) was placed unde1 endoscopic and fluoroscopic guidance. Distal stent migration was prevented by the acute angu- lation, causing a stricture-effect below the proximal flare. Proximal migration was prevented by](https://figures.academia-assets.com/72315061/figure_005.jpg)






![[653A] Barium swallow showing extrinsic compression. Purpose: Mediastinal granulomas are fibrocaseous masses usually found in association with fungal infections such as histoplasma. Esophageal involvement secondary to mediastinal histoplasmosis is rare and reported in 5-13% of cases. We present 22-year-old female recently relocated from Indiana with no medical history who complained of dysphagia to solid foods of 4 months duration. She denied fever, weight loss, odynophagia, hemetemesis or melena. She denied smoking, alcohol, or illicit drug abuse. Family history was positive for Non Hodgkin's Lymphoma in mother and maternal grandfather. Physical exam was normal. Initial labs: CBC, CMP, lactate dehydrogenase, vitamin D, and ACE level were normal. Barium esophagogram](https://figures.academia-assets.com/72315061/figure_012.jpg)
![{653B] CT chest showing enlarged lymph node with central calcification.](https://figures.academia-assets.com/72315061/figure_013.jpg)
![[654] Distal esophagus with melanoma metastases. Introduction: Metastatic malignant melanoma of the esophagus is a very rare disease. Since 1985, only 11 cases of metastatic malignant melanoma of esophagus have been reported1. We report another case of this type.](https://figures.academia-assets.com/72315061/figure_014.jpg)
![[658A] Upper endoscopy demonstrating esophageal mass. Purpose: Most patients with esophageal cancer present with dysphagia, odynophagia and/or weight loss. We describe an unusual presentation of esophageal cancer. A previously healthy 58-year-old female presented to the clinic with acute onset of obstructive jaundice. Laboratory work-up for viral, autoimmune and metabolic causes of liver disease was negative. Abdominal ultrasound and, subsequently, CT chest/abdomen/pelvis showed extensive thrombosis involving the left hepatic vein, intra- and extra-hepatic portal veins, superior mesenteric vein and splenic vein, along with extensive bilateral pulmonary emboli. There was no evidence of malignancy. She was then](https://figures.academia-assets.com/72315061/figure_015.jpg)
![[658B] CT abdomen demonstrating portal vein thrombosis.](https://figures.academia-assets.com/72315061/figure_016.jpg)


![[662] Normal upper esophageal sphincter.](https://figures.academia-assets.com/72315061/figure_019.jpg)




![{665] Linear columns of frond-like nodules in distal esophagus. increasing in frequency and severity over the past 6 months. He could not identify other incit ing factors. Bismuth suspension provided no relief. His alcohol intake had increased during thi: time (from 2 to 7 drinks per week), but he denied similar pain in the past, and denied tobacco fever, chills, nausea, vomiting, difficult or painful swallowing, abdominal distention, diarrhea constipation, rectal bleeding, black stool, or weight loss. His abdominal exam was benign withou tenderness. Hemoglobin was normal. He underwent upper endoscopy (EGD) for investigation EGD revealed linear columns of frond-like 8-10 mm nodules in the esophagus from 35-40 cm Pathology demonstrated superficial fragments of squamous papilloma without evidence of dys plasia or carcinoma. In-situ hybridization for low- and high-risk HPV subtypes was negative ESP is most often found incidentally on EGD in the distal esophagus. Risk factors include HPV infection, heavy alcohol use, and tobacco use. Pathogenesis is thought to be related to chroni inflammation. ESP was considered an entirely benign condition with some cases of spontane ous regression of lesions. More recent case reports, however, describe malignant transformation Despite this possible risk, the rarity of ESP precludes therapeutic or surveillance recommenda tions. Our patient’s (unrelated) abdominal pain improved on a proton pump inhibitor. Repea EGD was scheduled in 6-12 months.](https://figures.academia-assets.com/72315061/figure_024.jpg)

![{673] Figure 1: Distal esophageal adenocarcinoma 1 year after restrictive bariatric surgery.](https://figures.academia-assets.com/72315061/figure_026.jpg)
![[676B] Pre-myotomy pressures. [676A] Myotomy extending 16 cm. Case description:The patient is a 65-year-old Caucasian obese female who presented with heart- burn and indigestion with episodes of nausea for about 3 years. Initially, she would get occasional](https://figures.academia-assets.com/72315061/figure_027.jpg)

![{677B] Figure 2. Esophagus on EGD. Purpose: A 57-year-old Caucasian man with a 60-pack-year tobacco history and HIV on antiret- roviral therapy (CD4 954 cells/mm’, undetectable viral load) presented with 3 weeks of frontal headache upon awakening and a single episode of diplopia. He denied gastrointestinal symptoms or weight loss. Physical exam and laboratory analysis were unremarkable. A MRI of the brain revealed multiple high-density lesions in both cerebral hemispheres and the cerebellum with vasogenic edema, obstructive hydrocephalus, and partial effacement of the fourth ventricle (Figure 1). A work-up for tuberculosis, syphilis, cryptococcosis, toxoplasmosis, and cysticercosis was negative. The patient was started on intravenous corticosteroids for cerebral edema. A chest CT was notable for mild circumferential wall thickening of the distal esophagus with no intra-abdominal lymph- adenopathy. He then underwent an esophagogastroduodenoscopy, which revealed a nodular, fri- able, non-obstructive 4-cm mass in the distal esophagus (Figure 2). Pathology showed moderately differentiated invasive adenocarcinoma in a background of intestinal metaplasia. The incidence of brain metastasis from esophageal cancer has been reported to be 1.5% in retrospective studies, with the brain rarely being the only site of distant disease. Our patient presented solely with neu- rologic symptoms. Only two other cases have been reported in which symptoms related to a brain lesion preceded the diagnosis of the esophageal primary. The mechanism of spread to the brain is](https://figures.academia-assets.com/72315061/figure_030.jpg)


![[682] Figure 1A: Barium swallow shows dilated esophagus but no extravasation of con- trast; B: CT of chest shows collection adjacent to esophagus.](https://figures.academia-assets.com/72315061/figure_033.jpg)
![[688B] Over-the-scope clip.](https://figures.academia-assets.com/72315061/figure_034.jpg)
![[688A] Stent-in-stent.](https://figures.academia-assets.com/72315061/figure_035.jpg)
![[689A] Figure 1. Esophageal protuberance with ulceration and arterial bleed due to Dieulafoy lesion. A Difficult Pill to Swallow](https://figures.academia-assets.com/72315061/figure_036.jpg)
![[689B] Figure 2. Post-endoscopic injection of epinephrine and clip placement.](https://figures.academia-assets.com/72315061/figure_037.jpg)
![[691A] Figure 1: Typical features of eosinophilic esophagitis: pale mucosa, stacked circular rings, linear furrows, microabscesses and narrowed lumen. Purpose: We highlight complications of untreated eosinophilic esophagitis. A 33-year-old African American male Army veteran presented 4 hours after acute onset of severe substernal chest pain associ-](https://figures.academia-assets.com/72315061/figure_038.jpg)
![[691B] Figure 2: Mid-esophageal ulcer, 4 cm, exposing the muscularis propria.](https://figures.academia-assets.com/72315061/figure_039.jpg)
![[692] CT image showing dilated esophagus filled with food debris and associated tra: cheal compression.](https://figures.academia-assets.com/72315061/figure_040.jpg)

![[702] Endoscopic views of mass and CK20 stain. Discussion: There have been only two documented case reports of colon adenocarcinoma metasta- sizing to the esophagus. One case was treated with surgical bypass and the second with irinotecan and cetuximab chemotherapy. Of the cases reported, the endoscopic presentation has varied from an esophageal stricture to small nodular lesions. We present this case of colonic adenocarcinoma with metastasis to the esophagus with an endoscopic appearance of a fungating, friable mass on EGD, which responded to systemic chemotherapy with FOLFOX. In the setting of known colorectal carcinoma and dysphagia, metastatic disease remains a rare possibility, warranting a high index of suspicion. The treatment approach is dictated by the status of the primary tumor as well as the extent of metastasis.](https://figures.academia-assets.com/72315061/figure_042.jpg)
![(704] Figurel. Case: A 54-year-old man came to the hospital with complaint of tearing sensation in his lower chest after he tried to force down a beefsteak, which he felt got stuck in his throat. He mentioned that he has had multiple episodes of food getting stuck in throat in the past but he was able to resolve all of those by himself using fluids. This time, he developed intense pain and tearing-like sensation in his abdomen followed by spontaneous hematemesis. His chest X-ray on presentation did not show any abnormality and blood work revealed 13% eosinophilia. He underwent upper endoscopy, which showed severe grade D erosive esophagitis and also a 3-cm linear deep tear in the esophageal mucosa (Figure 1) involving the mid-esophagus with marked inflammation around it. There was no active bleeding. CT scan of chest was done, which showed pleural effusion and extra luminal air on the right side. He was managed conservatively with complete bowel rest and broad-spectrum intravenous antibiotics. The patient left against medical advice in less than 48 hours after admission. He was contacted 3 months later and he has been doing fine except for the persistent dysphagia.](https://figures.academia-assets.com/72315061/figure_043.jpg)



![[709B] Esophagus. [709A] See the metal hook.](https://figures.academia-assets.com/72315061/figure_047.jpg)
![[709C] Partial dentures pushed into stomach using upper scope.](https://figures.academia-assets.com/72315061/figure_048.jpg)

![[713] Atrial diverticulum in the circle. Purpose: We are reporting a case of upper GI bleed in a patient with atrioesophageal fistula where EGD could have been fatal. This case also underlines the importance of complete procedural his- tory in patients with GI bleed. A 57-year-old male with hypertension, dyslipidemia, and atrial fibrillation on rivaroxaban presented with chest pain, dyspnea on exertion, and one episode of coffee ground emesis. He was hemodynamically stable on admission with a normal CBC and BMP. Hemoglobin was 13.5 g/dL. He suddenly experienced an episode of severe chest pain and went into PEA arrest. He was resuscitated, intubated, and placed on a mechanical ventilator. NG was placed and 300 mL red blood was aspirated. Patient went into coma, but vital signs and remaining exam was normal. CT head revealed pneumocephalus and multiple cerebral infarcts. Repeat hemo- globin was 12.2 g/dL. EGD was not performed. Blood culture grew S. aureus and Strep. viridians. Later on it was found that he had catheter ablation for atrial fibrillation 18 days ago. Left atrial- esophageal fistula was suspected. CTA thorax showed a 5-mm posterior left atrial diverticulum raising a suspicion of pseudoaneurysm. A fistula between the esophagus and left atrium was found intra-operatively and it was repaired. Patient showed no neurological improvement and remained in coma, so life support was withdrawn after 11 days and patient died. Atrioesophageal fistula (AEF) is a rare complication of A Fib catheter ablation procedures, incidence rate 0.2%. It is associated with high mortality rate (70%). It can present 1-6 weeks after the ablation. Presenta- tion is nonspecific: fever, neurological deficits, and chest pain. None of the previously reported cases described GI bleeding symptoms. EGD can cause fatal air-embolism so it should be avoided. CT chest can help to establish diagnosis. Surgery can be lifesaving. AEF should always be on the differential diagnoses of UGI bleeding in appropriate setting: unexplained fever and neurological deficit after recent ablation procedure.](https://figures.academia-assets.com/72315061/figure_050.jpg)
![[717] Barrett’s metaplasia arising from gastric heterotopia. Purpose: A gastric inlet patch (GIP), also known as a cervical inlet patch or gastric heterotopia, is a discrete island of columnar mucosa found in the cervical esophagus. Its origin may be congeni- tal or acquired. GIPs are seen in up to 10% of patients on upper endoscopy. Although most GIPs are asymptomatic, some patients present with dysphagia, globus sensation, or even reflux. These symptoms may arise from GIPs with oxyntic acid-secreting mucosa. Cases of high-grade dyspla- sia and adenocarcinoma arising from GIPs have been reported. However, there are no published reports confirming the presence of Barrett’s metaplasia arising from a GIP. A 46-year-old woman presented for evaluation of multiple gastrointestinal complaints. Her greatest concern was “reflux” that worsened during each day. She also noted dysphagia to solid foods and rare odynophagia. Evaluation included esophageal manometry, which demonstrated elevated lower esophageal sphinc- ter pressures with normal amplitude peristalsis. Upper endoscopy identified 2 rectangular-shaped salmon-colored patches in the cervical esophagus, each measuring 1 x 1.5 cm. Biopsies showed squamoglandular oxyntic mucosa with intestinal metaplasia, consistent with Barrett's esophagus, as well as reflux esophagitis. Forty-eight hour pH testing off PPI confirmed increased acid exposure to the distal esophagus, but only mild reflux esophagitis with no Barrett’s metaplasia seen on biopsies of this region. Given her symptoms and endoscopic findings, treatment of the GIPs was planned. Two sessions of focal radiofrequency ablation (RFA) were performed using the Halo” device (Covi- dien GI Solutions, Sunnyvale, CA), resulting in complete endoscopic eradication of both GIPs. Post- ablation biopsies confirmed the absence of gastric heterotopia and Barrett’s metaplasia. The patient noted complete resolution of her symptoms, even after stopping proton pump inhibitors. To our knowledge, this is the first case with biopsy-proven Barrett's metaplasia found to arise from a GIP.](https://figures.academia-assets.com/72315061/figure_051.jpg)



![[727] Recurrent tumor before LN2SC (A), after 3 treatments (B), and after 2 years of palliation (C).](https://figures.academia-assets.com/72315061/figure_054.jpg)
![[733B] Axial CT demonstrating gastric pneumatosis (circle). [733A] Axial CT demonstrating air in portal vein (circle).](https://figures.academia-assets.com/72315061/figure_055.jpg)

![{734B] CT Scan showing hiatal hernia. [734A] CXR showing hiatal hernia.](https://figures.academia-assets.com/72315061/figure_057.jpg)




![[741] Gastric emptying study results](https://figures.academia-assets.com/72315061/table_003.jpg)
![[746] Figure 1: A. Retroflexed view of the lesser curve gastric hematoma / tear (arrow) B. CT-gastric hematoma (arrow). C. Tearing on insufflation. D. Biopsy-Congo Rec stain. Discussion: Incidence of AL amyloidosis in the U.S. is 6-10 cases per million person- years, with 10-15% of multiple myeloma patients having AL amyloid. Only 1% have symp- toms from gastric involved AL amyloidosis. Patients can present with peri-orbital pinch purpura. Endoscopic features include ulcerations, granular and friable mucosa, irregular gastric folds, submucosal hemorrhage, and hematomas. Bleeding in AL amyloidosis is due to capillary fragility from amyloid deposition, coagulation factor deficiency, especially low factor X, and abnormal platelets. The goal of therapy is to suppress the synthesis of light chains by treating the underlying disorder.](https://figures.academia-assets.com/72315061/figure_062.jpg)
![[750] Hypertrophic gastric folds. Purpose: We present a 59-year-old male with a history of hypertension, Helicobacter pylori infec- tion two years prior to admission status post triple therapy who presented with bilateral lower extremity edema that had become excruciatingly painful 2 weeks prior to his admission. On exam, he was cachetic with temporal wasting. He had no jugular venous distention and his lungs were clear. Abdominal exam was significant for tenderness in the epigastrium. Murphy’s sign was negative. There were no appreciable abdominal masses, and stool guaiac was negative. He had 4+ bilateral pitting edema in the lower extremities. Hemoglobin was 7.6g/dl with an MCV of 70.6 fl. Kidney and liver function tests were unremarkable. Albumin was 2.6g/dl. Brain natriuretic](https://figures.academia-assets.com/72315061/figure_063.jpg)
![[751] Massively dilated stomach measuring 33.1 x 12.8 x 11.3 cm. Conclusion: Acute gastric dilatation is a rare and poorly understood condition. Complications including gastric perforation have been attributed to elevated intra-gastric pressure. There is a well documented association with anorexia/bulimia nervosa. Our case of acute gastric dilation in a malnourished patient with ulcerative colitis suggests that co-existing malnutrition may contribute to the pathogenesis of this entity. We also highlight the importance of nasogastric decompression.](https://figures.academia-assets.com/72315061/figure_064.jpg)
![[752A] Figure 1. Initial EUS of gastric mass. Purpose: Accessory spleens are an asymptomatic, develop from residual tissue following a sple- nectomy and found incidentally. A 58-year old male went to his PCP for complaints of consti- pation. The patient’s PMH includes left nephrectomy and splenectomy secondary to a MVA. Previous EGD showed a lesion in the fundus of the stomach. He was transferred to our hospi- tal for EUS (Figure 1). Sonographically, the lesion appeared to originate from the muscularis propria. Surgical pathology was diagnostic for accessory spleen (Figures 2). Accessory spleens can mimic abdominal tumors. On ultrasound, it appears as a round or oval mass with a mildly echogenic and homogenous texture; CT and MRI it appears as the same density as the spleen. EUS is a better modality for differentiating between an externally compressing lesion and a sub- mucosal tumor.](https://figures.academia-assets.com/72315061/figure_065.jpg)
![[752B] Figure 2. EGD view of gastric mass.](https://figures.academia-assets.com/72315061/figure_066.jpg)
![[752C] Figure 3. Surgical pathology slide.](https://figures.academia-assets.com/72315061/figure_067.jpg)
![[752D] Figure 4. Surgical pathology.](https://figures.academia-assets.com/72315061/figure_068.jpg)
![[754] Image showing three pyloric openings into duodenal bulb.](https://figures.academia-assets.com/72315061/figure_069.jpg)



![[759A] Firm antral submucosal mass. Conclusion: Gastric schwannomas are a rare benign tumor of the gastrointestinal tract. The endo- sonographic features mimic the appearance of gastrointestinal stromal tumors. The hypocellular- ity of the fine needle aspirate further complicates identification of this tumor prior to surgical resection.](https://figures.academia-assets.com/72315061/figure_073.jpg)
![[759B] FNA of submucosal lesion.](https://figures.academia-assets.com/72315061/figure_074.jpg)




![[767A] H&E illustrating anaplastic GIST.](https://figures.academia-assets.com/72315061/figure_079.jpg)
![[767C] MRI of a 6.8 x 7.7 cm complex splenic mass and a hepatic cyst.](https://figures.academia-assets.com/72315061/figure_080.jpg)
![{767B] Immunohistochemical staining of the spleen indicating c-kit/ CD117 negative GIST.](https://figures.academia-assets.com/72315061/figure_081.jpg)

![[772] Nodular gastritis. Purpose: Kaposi's sarcoma (KS) was a rare neoplasm that comprised close to 0.1% of all malignancies worldwide. However, due to the increasing prevalence of patients with human immunodeficiency](https://figures.academia-assets.com/72315061/figure_083.jpg)

![[773] Semi- circumferential hemorrhagic gastropathy. Conclusion: Post-TACE hemorrhagic erosive gastropathy is a rare but potentially serious complica- tion and is often due to non-target arterial embolization. Preoperative angiography may outline arterial variants and allows for superselective embolization. Discussion: Peri and post-procedural complications occur in approximately 10% of patients under- going TACE. GI bleeding occurs in less than 1%. It is usually related to preexisting pathology or directly related to the procedure. Possible risk factors include prior history of portal gastropathy/ varices, peptic ulcer disease, or direct toxicity of administered embolizing or chemotherapeutic agents. Bleeding under these circumstances is often delayed for days after the procedure. Rarely, an ischemic injury may be precipitated from emobolizing small nontarget arterial branches of the hepatic artery. This type of non-target arterial injury may be predicted from the pre-operative angio- graphy, and typically induces bleeding during the early post-operative period, as in this case. Conclusion: Post-TACE hemorrhagic erosive gastropathy is a rare but potentially serious complica-](https://figures.academia-assets.com/72315061/figure_085.jpg)

![[777] Figure 1. EUS demonstrating a hypoechoic, oval shaped, gastric body mass. Case Presentation: A 66 year-old man with history of stage III squamous cell lung carcinoma presented with dyspnea and cough. The patient had known regional lymph node metastatic disease but no distant metastases. During his emergency department evaluation, a CT of the chest demonstrated a 5.7 cm x 4.7 cm mass in the greater curvature of the stomach. Of note, lower cuts of a prior CT scan of the chest 4 months previous had not shown any gastric mass. On EUS, an oval intramural, subepithelial 5.8 cm x 4.2 cm lesion was found in the greater curvature of the stomach 7 cm distal to the gastroesophageal junction. The lesion was hypoechoic, homo- geneous and extended from the submucosal layer to the serosa. There was an intact echo-interface seen between the mass and the liver and celiac trunk (Figure 1). Transgastric FNA using a 22g needle revealed metastatic keratinizing squamous cell carcinoma (immunostains positive with cytokeratin AE1/3, p63 and negative with CD117, cytokeratin 7; equivocal staining with DOG-1). A PET-CT](https://figures.academia-assets.com/72315061/figure_087.jpg)

![[782B] Figure 2.](https://figures.academia-assets.com/72315061/figure_089.jpg)
![[782A] Figure 1. Purpose: Schwannoma is a rare gastrointestinal mesenchymal tumor comprised of encapsulated nerve sheaths most commonly found in the stomach. Usual presentation is epigastric discomfort and/or bleeding. Although gastric schwannomas are usually benign, malignant transformation has been reported. A 72 year old Caucasian female presented to our institution with 3 days of melena with associated epigastric pain in the setting of anticoagulation with warfarin. The patient under- went urgent endoscopy after correction of coagulopathy and hemodynamic resuscitation, which revealed a 2.5 - 3 cm submucosal mass along the greater curvature of the body of the stomach with a clean-based 8 mm ulceration (Figure 1). Biopsies were taken with resultant pathology being non- diagnostic. Imaging revealed a 3.2 x 2-cm solid mass within the body of the stomach (Figure 2). No evidence of perigastric lymphadenopathy or metastatic disease was noted. The patient underwent laparoscopic partial gastrectomy with wedge resection of the mass. The tumor consisted of a well- circumscribed proliferation of spindle cells with approximately 1 mitotic figure per 50 high power fields. The tumor stained strongly with S-100 and GFAP and was negative for DOG-1, CD117, CD34, smooth muscle actin, and CD57. These histological and immunohistochemical findings were diagnostic of a schwannoma. Most instances of upper gastrointestinal bleeding from a submucosal mass are from GIST tumors; however, schwannomas must be considered in the differential. Despite published CT characteristics of schwannomas, differentiation between other submucosal masses is difficult. Complete resection is usually curative and malignant transformation is rare. In this case, the patient did well and was discharged home on postoperative day 4. No additional treatment is planned.](https://figures.academia-assets.com/72315061/figure_090.jpg)

![[785] H & E Stain. Helicobacter heilmannii are significantly larger in size and a more tightly coiled appearance than Helicobacter pylori.](https://figures.academia-assets.com/72315061/figure_092.jpg)
![[787] LNA 1 immunostain. Background: Kaposi’s sarcoma (KS) is a low grade vascular tumor. In the United States, the major- ity of affected patients have human immunodeficiency virus infection. It is the most common acquired immunodeficiency syndrome associated malignancy. Skin lesions are typical features with visceral organ involvement occurring less commonly. Gastrointestinal tract (GI) KS is usu- ally asymptomatic and often unrecognized in clinical practice. In this case, we present a patient](https://figures.academia-assets.com/72315061/figure_093.jpg)




![[796] Figure 2. Histopathology revealing foveolar hyperplasia, vascular ectasia, granula- tion tissue, and scattered selective internal yttrium 90-labeled radiation microspheres. Purpose: Colon cancer (CRC) is one of the most common cancers in the world. Although sur- gical resection with neoadjuvant therapy is effective in most patients, some develop unresectable metastatic disease, commonly to the liver. One novel approach, selective internal radiation therapy (SIRT) with yttrium 90-labeled microspheres (Y-90), administered via hepatic artery branches, is a method used to selectively deliver radiation therapy to inoperable liver metastases. A few reports have shown benefit. However, there have been reports where microspheres get caught in the gastric and duodenal capillary beds leading to complications. We report herein a case of selective inter- nal radiation (SIR)-microsphere-induced gastritis. A 66-year-old woman was diagnosed with CRC in 2010. Imaging demonstrated a right colonic mass and liver metastases. She underwent right hemicolectomy with neoadjuvant chemotherapy. She subsequently underwent SIRT with Y-90 in 2011. Several weeks after therapy, she developed abdominal pain and progressive weight loss. An esophagogastroduodenoscopy (EGD) revealed gastric ulcers. Pathology revealed foveolar hyper- plasia, vascular ectasia, granulation tissue, and scattered Y-90 microspheres (Figure). Treatment with proton pump inhibitors (PPIs), carafate, and misoprostol did not provide benefit. Hyperbaric oxygen therapy was considered. The liver represents the most common site of metastases of CRC. Although surgical resection of solitary liver metastases can result in long-term survival, not all patients are candidates for surgery. For those patients, chemotherapy or other modalities including SIRT with Y-90 become options. However, retrograde migration of the microspheres into the gastric or duodenal circulation may occur. This can cause ulceration of the stomach and the duodenum. Treatment options include PPIs, carafate, misoprostol and hyperbaric oxygen therapy. With the anticipated increase in use of SIRT for hepatic malignancy treatment, clinicians should be aware of the potential for gastrointestinal complications from retrograde migration of Y-90 microspheres into the gastroduodenal circulation.](https://figures.academia-assets.com/72315061/figure_097.jpg)
![[797C] Figure 3. The cytomegaloviral (CMV) gastritis demonstrates a granuloma, com- prised of aggregated epithelioid histiocytes with admixed lymphocytes, plasma cells, and eosinophils; there is associated foveolar injury (hematoxylin and eosin, high mag- nification). {797B] Figure 2. The cell with viral cytopathic effect (as shown in figure 1) shows nuclear-pattern immunoreactivity for cytomegalovirus (CMV) (immunostain for CMV, high magnification).](https://figures.academia-assets.com/72315061/figure_098.jpg)
![[797A] Figure 1. The antral gastritis is characterized by a lymphoplasmacytic infiltrate with neutrophilic component, few eosinophils, and foveolar/pit injury; as indicated by the arrow, a pit epithelial cell shows classic cytomegalovirus-induced cytopathic effect, characterized by cell enlargement and a large intranuclear eosinophilic inclusion with surrounding halo (hematoxylin and eosin, intermediate and high magnifications, respectively).](https://figures.academia-assets.com/72315061/figure_099.jpg)


![[809] EUS-guided fine-needle aspiration of the pancreas,shows an exclusive popula- tion of small lymphocytic cells. Case Report: We report a 69-year-old female with history of chronic lymphocytic leukemia (CLL)/ small lymphocytic lymphoma with breast involvement, who presented with one-day history of acute abdominal pain associated with nausea and vomiting. The patient had experienced multiple episodes of acute pancreatitis in the past without clear etiology. On examination, she had mild epigastric ten- derness without organomegaly. Laboratory data showed lipase of 849 unit/L, amylase of 126 unit/L, hematocrit of 36.8, white blood cells count of 20,000 with 76% lymphocytes and moderate amount of smudge cells. Abdominal ultrasound was performed with limited results due to overlying bowl gas. Abdominal computerized tomography revealed mild splenomegaly with no intraabdominal masses or lymphadenopathy. Endoscopic ultrasonography (EUS) discovered multiple masses in the body/tail junction of the pancreas with the largest size of two centimeters. No stones or ductal filling defects were detected. EUS-guided fine-needle aspiration of the largest pancreatic mass was performed, which revealed a population of exclusive small lymphocytic cells likely small lymphocytic lymphoma. Given her history of CLL, the diagnosis of secondary CLL of the pancreas was rendered. Conclusion: Even though recurrent acute pancreatitis is an extremely rare presentation of secondary pancreatic lympho- proliferative lesions, physicians should be aware of this condition as a cause of recurrent pancreatitis, especially in patients with known history of CLL/SLL. The diagnosis of these disorders requires patho- logic confirmation to distinguish lymphoma from other tumors or autoimmune processes.](https://figures.academia-assets.com/72315061/figure_102.jpg)




![[811B] Lymph node biopsy.](https://figures.academia-assets.com/72315061/figure_107.jpg)
![[814] CT scan abdomen showing pancreatic tail mass invading to colon and spleen, also shown liver lesions.](https://figures.academia-assets.com/72315061/figure_108.jpg)
![[816] CT abdomen showing dilated intrahepatic duct and presence of biloma. jaundice, right upper quadrant tenderness. Labs: T. bilirubin 10.6, direct bili 8.3, AST/ALT 130/265, alk phos 361, normal INR & CBC. CT abdomen showed intrahepatic biliary dilation. She underwent unsuccessful ERCP with inability to cannulate common bile duct. Percutaneous 8.5 French biliary drain was placed with improvement in bilirubin and symptoms on discharge. She returned 2 weeks later with hemetemesis, bile leak from the site of percutaneous drain and right upper quadrant pain. T. bilirubin 11.5, AST/ALT 146/195, alk phos 850, Hb 8.2, which was 11.2 two weeks ago. Repeat CT abdomen showed right sub-diaphragmatic fluid collection consistent with biloma. Tagged red blood cell scan and EGD were negative. Transhepatic cholangiogram showed dye extravasation into biloma, distal drain](https://figures.academia-assets.com/72315061/figure_109.jpg)
![[818] MRI: abnormal foci of ill-defined signal and enhancement in both kidneys, anc pancreas.](https://figures.academia-assets.com/72315061/figure_110.jpg)
![[823] Polyp prolapsing into the second part of the duodenum; gross and endoscopic sonogram.](https://figures.academia-assets.com/72315061/figure_112.jpg)
![[824B] SpyGlass™ cystic duct stone.](https://figures.academia-assets.com/72315061/figure_113.jpg)


![[828] Pancreatic hemorrhage. Discussion: Rivaroxaban is an orally available direct factor X inhibitor, recently approved by the FDA. Its primary benefit over prior forms of anticoagulation is its ability to provide convenient oral anticoagulation, without the need to monitor levels. Studies comparing this agent to older forms of anticoagulation have demonstrated increased risks for critical bleeding and need for transfusion, most commonly from the GI tract or intracranial hemorrhage. The lack of a clinically proven reversal agent has also been a cause for concern. While spontaneous bleeding when taking this medication may rarely occur, its occurrence in this patient with no history of trauma raised suspicion for underlying pathology. This suspicion was confirmed on the follow-up CT scan, which documented a pancreatic mass. This case is notable for a novel pancreatic source of major bleeding in a patient on rivaroxaban, as well as a clinically significant improvement upon adminis- tration of profilnine SD. Spontaneous pancreatic hemorrhage or hemoperitoneum while on rivar- oxaban should raise suspicion for an underlying pancreatic pathology including pancreatic tumors.](https://figures.academia-assets.com/72315061/figure_116.jpg)


![[833] CT scan before and after irradiation and CT simulation before radiation treatment.](https://figures.academia-assets.com/72315061/figure_119.jpg)
![[837] Contrast enhanced CT scan of abdomen showing a cystic lesion in the pancreatic tail extending into the spleen (arrowhead).](https://figures.academia-assets.com/72315061/figure_120.jpg)


![[850] Fluoroscopic image showing proximal CBD stricture; endoscopic image showing SEMS.](https://figures.academia-assets.com/72315061/figure_123.jpg)
![[855] Fistulous tract between pancreas and stomach on CT and endoscopy. Purpose: To identify pancreatogastric fistula as a rare complication of necrotizing pancreatitis presenting as hematemesis and melena. Case: A 48-year-old male with history of alcohol abuse presented with severe epigastric pain for 5 days. He also reported six episodes of hematemesis and associated melena which started 24 hours prior to presentation. He denied fever or chills. On admis- sion, he was hypotensive (96/62), tachycardic (107), afebrile (98.3 F) with epigastric tenderness and maroon stool in rectal vault. Hbg dropped from 7.7 g/dL to 4.8 g/dL. WBC count was 22.1 K/mm* and lipase was 16 U/L. A CT scan showed chronic pancreatitis and pancreatic pseudocyst abating the stomach. EGD showed clotted blood in the entire stomach but no site of active bleeding was identified. A large fistula leading to pseudocyst was found in the cardia noted to be draining pus and debris. The cyst was accessed by the gastroscope for possible irrigation and debridement. However, bleeding of arterial nature appeared from within the cyst that could not be stopped despite epineph- rine injections and the procedure was aborted. A tagged RBC scan showed no evidence of active bleed suggesting that bleeding had ceased. In the absence of active bleed and ongoing necrotizing and inflammatory process emergent surgical intervention was deferred and he was monitored in the ICU. His Hbg remained stable requiring no further transfusions. Patient was pain-free and tolerat- ing regular diet at day 3 of hospitalization. A CT was done that showed reduction of cyst size to less than half within a week of initial presentation. Discussion: Fistula formation is one of the most feared complications of pancreatitis. Secondary to close proximity, fistula in most cases connects the pseudocyst to either the transverse colon or splenic flexure, but in our patient, it formed between a pseudocyst and the stomach. A study by G.G. Tsiotos, et al evaluating the incidence of fistula forma- tion following necrotizing pancreatitis showed that none of the 64 patients had gastropancreatitic fistula prior to surgery. The inflammatory process which results in fistula formation can also lead to vascular invasion and in the presence of communication with GI lumen and the patient can present with hematemesis and melena, which can be misleading. Fistula by providing a drainage path can facilitate healing.](https://figures.academia-assets.com/72315061/figure_125.jpg)

![[862] Figure 1. Endoscopic retrograde cholangiopancreatography demonstrating multiple intrahepatic segmental strictures and dilations.](https://figures.academia-assets.com/72315061/figure_127.jpg)


![[868] ERCP image: cystic duct filling defect.](https://figures.academia-assets.com/72315061/figure_130.jpg)


![[882] Extracted daughter cyst wall. Discussion: Hepatic hydatid cysts are usually asymptomatic. Symptoms occur due to the size of the cyst causing pressure on the liver parenchyma or from possible intrabiliary rupture. Intrabili- ary rupture can occur occultly when the cystic fluid only drains into the biliary tree or as a frank rupture with intracystic material and/or daughter cysts draining into the biliary tract. ERC per- formed preoperatively in a patient with hydatid cyst with or without biliary dilation may avoid an unnecessary CBD exploration. It can be used for definition of biliary anatomy providing a roadmap of cystobiliary fistulas prior to cystectomy. Additionally, daughter cysts may be extracted from the](https://figures.academia-assets.com/72315061/figure_132.jpg)

![[894] ERCP showing pancreatic divisum.](https://figures.academia-assets.com/72315061/figure_134.jpg)
![[897A] CBD filling defect.](https://figures.academia-assets.com/72315061/figure_135.jpg)
![[897B] Polypoid tissue within CBD.](https://figures.academia-assets.com/72315061/figure_136.jpg)
![[903] Sclerosing cholangitis. Conclusion: AIDS cholangiopathy classically presents with intrahepatic sclerosing cholangitis and ampullary stenosis. Treatment is primarily endoscopic, with biliary sphincterotomy in cases with ampullary stenosis. Eradication of the viral or protozoal infection does not influence symptoms or chol- angiographic abnormalities.](https://figures.academia-assets.com/72315061/figure_137.jpg)

![[905] Figure 1. T2 image showing enhancing 2.8 cm mass in the body of pan- creas with an additional lesion in tail (not shown in this image) and otherwise normal looking pancreas. Discussion: Metastatic pancreatic disease constitutes about 2% of all pancreatic malignancies. There are very few reports about pancreatic metastases from LMS. Although the pancreas is a retroperitoneal organ and is located in close proximity to the primary lesion, the above case demonstrates unpredictable lesion characteristics, with pancreatic metastases occurring nearly 9 years after primary diagnosis succeeding metastases to distant regions like lungs and lower extremities. A high index of suspicion is needed with unusual pancreatic findings in patients with other primary malignancies. When feasible, surgical exci- sion of the pancreatic metastases is an effective treatment strategy. The report highlights the utility of EUS to detect and diagnose metastatic lesions to the pancreas.](https://figures.academia-assets.com/72315061/figure_138.jpg)
![[907] Figure 1. FNA of the nodules in pancreatic head performed through an avas: cular plane.](https://figures.academia-assets.com/72315061/figure_139.jpg)

![[911] EUS view of the pancreatic neck mass. abnormal soft tissue along the retroperitoneum encasing the celiac axis origin and the superior mes- enteric artery. There was also presence of splenic vein occlusion with numerous left upper quadrant varices, as well as diffuse biliary ductal dilatation with a transition point near the level of the ampulla. At this time, surgical pathology resulted as a moderately differentiated adenocarcinoma extending through the bowel wall into the subserosa, but sparing the mucosal layer, suggesting it was metastatic. EUS was performed and revealed a large hypoechoic mass in the neck of the pancreas measuring 2.3 x 2.4 cm with involvement of the celiac and superior mesenteric arteries. Both the mass and a large celiac lymph node were biopsied, and FNA cytology confirmed pancreatic adenocarcinoma within both. This is a rare presentation of metastatic pancreatic adenocarcinoma with metastasis to the sigmoid colon presenting as a large bowel obstruction.](https://figures.academia-assets.com/72315061/figure_141.jpg)
![[912] Proximally migrated pancreatic duct stent as seen on endoscopic retrograde pancreatogram. Purpose: A 43-year-old Caucasian woman with a medical history significant for obesity was evaluated for intermittent right upper quadrant abdominal pain for several months. Abdominal ultrasound showed gallstones and a dilated common bile duct of 9 mm. Laboratory studies showed elevated transami- nases. An initial endoscopic retrograde cholangiopancreatogram (ERCP) was performed for suspected](https://figures.academia-assets.com/72315061/figure_142.jpg)
![[916A] The ruptured SAPA as seen on EGD with overlying fibrin clot. Purpose: A 44-year-old man with past medical history of alcohol abuse presented to the ER with a com- plaint of three episodes of hematemesis and two episodes of syncope in the 2 days preceding presenta- tion. Initial hemoglobin was 3.5 mg/dL, heart rate was 120 beats per minute, and systolic blood pressure was approximately 70 mm/Hg. Emergent EGD displayed what appeared to be a gastric varix with overly- ing fibrin clot. CT of the abdomen displayed chronic pancreatitis and a splenic artery pseudoaneurysm (SAPA). The patient underwent CT angiography and the SAPA was treated via transcatheter arterial embolization (TAE). Only 160 cases of SAPA have been reported in the literature. Chronic pancreatitis is the leading etiology. Rupture of a SAPA can lead to rapid exsanguination and is associated with 90% mortality rate when untreated. EGD remains the procedure of choice in a patient with hematemesis; however, a SAPA is not likely to be visible on EGD. Our case is unique in that the SAPA was immediately visible on EGD. This case champions the early use of CT angiography when EGD can not elicit the cause of upper GI bleeding. Prior to the advent of interventional radiology, surgery was the only treatment for SAPA. Currently, TAE is the recommended treatment for those patients who are hemodynamically stable enough to undergo the procedure. The success rate for management of a SAPA with TAE is approxi- mately 85% and carries a minimal risk of complication. Size of the SAPA has not been shown to be a determinant of likelihood of rupture; thus, when discovered, a SAPA warrants treatment regardless of size or symptoms.](https://figures.academia-assets.com/72315061/figure_143.jpg)
![[916B] The SAPA as seen on CT angiography.](https://figures.academia-assets.com/72315061/figure_144.jpg)
![[919A] Biopsy of the mass in the common bile duct; red arrow showing squamous cells with keratinization and intracellular bridging, consistent with squamous cell carcinoma. Purpose: Primary squamous cell carcinoma is a rare and a very aggressive form of carcinoma of the gallbladder. We have recently seen a 63-year-old man, a chronic smoker, with an aggressive squamous cell gallbladder cancer, presenting with obstructive jaundice. He underwent CT scan and was found to have a mass engulfing the entire gallbladder, with extensive local invasion to the liver and bile ducts. Histology from ERCP-guided biopsy of CBD and CT-guided biopsy the liver mass confirmed the diagnosis of pure squamous cell cancer. The patient underwent ERCP and biliary stent placement, leading to improve- ment in clinical status and cholestatic jaundice. Squamous metaplasia, or squamous cell differentiation of preexisting adenocarcinoma, are believed to be the most acceptable hypotheses to explain the existence](https://figures.academia-assets.com/72315061/figure_145.jpg)

![[920A] SB video capsule endoscopic picture revealing ileal edema and narrowing. Case Report: A 70-year-old male presented with iron deficiency anemia. He complained of diarrhea, and colonoscopy results from five months earlier was normal to the cecum, with ileal intubation. Colon biop- sies were negative for microscopic colitis. The patient then presented with severe fatigue, and bloodwork revealed microcytic anemia and a HgB = 10.4 gm % (N=12-16). Given that the patient had undergone a](https://figures.academia-assets.com/72315061/figure_147.jpg)
![[920B] Axial non-contrast CT of the abdomen demonstrating a 3.6 cm spiculated mesenteric mass with desmoplastic reaction (red circle). Conclusion: Metastatic neuroendocrine tumor of the ileum can present with iron deficiency anemia. SB video capsule endoscopy was helpful in diagnosing this disorder.](https://figures.academia-assets.com/72315061/figure_148.jpg)
![[922] Chronic inflammatory cell infiltrates and foci of brown-black pigment in lamina propria consistent with melanosis in duodenum. Conclusions: Melanosis duodeni: endoscopically seen as discrete, flat, small, brown-black dark pig- mented spots in the duodenal mucosa, and is generally considered to be local deposition of iron from oral iron intake. There is no known association with pigmentation elsewhere in the GI tract, or with the use of laxatives. On literature review, the exact mechanism is unknown; it is found to be associated with history of oral iron intake, upper GI bleeding, co-morbid conditions like HTN, ESRD, CHF, DM and certain medications like hydralazine or diuretics, most of which were present in our case. Although it is a benign condition of unclear clinical importance that does not require any specific therapy, endoscopists and pathologists must be aware of this rare entity.](https://figures.academia-assets.com/72315061/figure_149.jpg)






![[930] Cross-sectional computed tomography view of the terminal ileum (intussuscep- tum) within the ascending colon (intussuscipens). Discussion: Adult intussusception is rare and it’s usually secondary to an underlying etiology or a leading point. It’s idiopathic in about 10% only. In the small intestine, it's mainly secondary to a benign etiology including benign neoplasms, adhesions, Meckel’s diverticulum, lymphoid hyperplasia, celiac disease,](https://figures.academia-assets.com/72315061/figure_156.jpg)
![[931A] Capsule endoscopy of small bowel telangiectasia. Case Report: A 67-year-old man presented with breathlessness, symptomatic anemia for 3-4 days and was found to have HB <7. He had no overt bleeding, abdominal pain, nausea and vomiting. He had a his- tory of repeated hospitalization for symptomatic anemia. He had 12 admissions in 10 months for symp- tomatic anemia and received 34 U of pecked RBC transfusion in 10 months. Physical examination was unremarkable except for marked pallor. Lab data were within the reference range except positive stool occult and low hemoglobin of 5.2 to 7.9 on every admission with iron deficiency anemia. He had multiple endoscopies, including four upper endoscopies, three colonoscopies, three enteroscopies and three 3 capsule endoscopies. EGD and colonoscopy on first admission showed AVM in esophagus, caecum and ascending colon and clipping was done. Capsule endoscopy showed multiple non-bleeding telengiecta- sia in jejunum and ileum. Treatment with push enteroscopy and endotherapy was recommended, and he had three push enteroscopies with endotherapy. However, he continued to require frequent admis- sion with blood transfusion, and he is not keen for further enteroscopic treatment. Therefore, octreotide 50 mcg bid was given as a last option. Result: After treatment with octreotide, our patient has no further episode of symptomatic anemia in 20 weeks follow up period, and his hemoglobin level is stable in the range of 9-9.5 g/dl.](https://figures.academia-assets.com/72315061/figure_157.jpg)
![(931B] Ileal A-V malformation.](https://figures.academia-assets.com/72315061/figure_158.jpg)
![GI Sarcoidosis (932] Figure 1. Case Report: 54-year-old female with no reported past medical history initially presented to an outside physician with complaint of sudden onset of abdominal pain and some associated nausea. CT scan of the abdomen revealed small bowel intussusception with a transition point in the proximal small bowel. Initial laboratory including hemoglobin was unremarkable. The patient underwent an endoscopy, which revealed diffuse moderately scalloped mucosa in the first through the third part of the duodenum](https://figures.academia-assets.com/72315061/figure_159.jpg)


![[936] Bread bag clip in the duodenal sweep. References: 1. Morrissey SK, Thakkar SJ, Weaver ML, Farah K. Bread bag clip ingestion: A Rare Cause of Upper Gastrointestinal Bleeding. Gastroenterol Hepatol 2008 July;4(7):499-500.](https://figures.academia-assets.com/72315061/figure_162.jpg)

![[938] Image 1. Actively bleeding 20-mm ulcer in the TI. Introduction: BD is characterized by recurrent oral and genital ulcers, uveitis and skin lesions. Preva- lence of BD is highest in countries along the ancient silk road. By comparison, prevalence in Western countries is rare: 1 per 15,000-500,000. The frequency of GI involvement amongst patients with BD is variable. Low frequency has been reported in Turkey (2.8-5%), moderate frequency in the USA (30%) and the highest frequency has been reported in Japan (50-60%). Ileocecal and colonic involvement are most commonly reported.](https://figures.academia-assets.com/72315061/figure_164.jpg)
![[947] Scalloping mucosa of the jejunum.](https://figures.academia-assets.com/72315061/figure_165.jpg)
![[950] Figure 1. Submucosal ulcerated polyp found approximately 180 cm from the pylorus with antegrade single balloon enteroscopy. Purpose: A 26-year-old woman presented with one-day history of hematochezia beginning shortly after undergoing dilation and evacuation for retained products of conception. On initial evaluation, the patient was hypotensive, tachycardic and acutely anemic (hemoglobin/hematocrit 8.6/25.5). An emergent CT scan with rectal contrast ruled out bowel or uterine injury. Urgent EGD and colonoscopy were performed, however, no sign or source of bleeding was identified. A tagged RBC scan showed only vaginal bleeding. The patient subsequently stabilized; however, two days later, she had recurrent hema- tochezia and worsening anemia with a hemoglobin of 6.4. She denied any vaginal bleeding at that time, having used a tampon to avoid confusion. Thus repeat EGD and colonoscopy were performed, which, again, did not identify a source of bleeding. However, a capsule endoscopy revealed fresh blood in the proximal to mid-small bowel. She thus underwent an urgent antegrade single balloon enteroscopy, where a 1.5-cm submucosal polyp with an ulcerated and necrotic surface was found at approximately 180 cm from the pylorus (Figure 1). The lesion was tattooed with India ink and injected with diluted epinephrine. A diagnostic laparoscopy with segmental small bowel resection removed the lesion and pathology of the polyp returned as intravascular papillary endothelial hyperplasia (Masson's tumor). Masson’s tumors are benign vascular lesions that arise from intravascular endothelial proliferation in the setting of thrombus. They primarily affect the extremities, head and neck and have rarely been described within the abdomi- nal cavity. To the best of our knowledge, only five other cases of Masson's tumor in the small bowel have been reported in the literature. When involving the GI tract, patients typically present with abdominal pain, melena, and anemia. The case described here is unique in that it is the only known instance of a patient with a Masson's tumor of the small bowel presenting with hematochezia.](https://figures.academia-assets.com/72315061/figure_166.jpg)

![955] Retroperitoneal mass with areas of necrosis and calcification. Conclusion: XGI in a retroperitoneal mass with tumor implants in the small bowel causing obstruc- tion has not previously been reported. Although rare, this case demonstrates that clinicians should be aware of the possibility for XGI to occur in the retroperitoneal space and the small bowel with subsequent SBO.](https://figures.academia-assets.com/72315061/figure_168.jpg)

![[970] Left image: hemoclip placed for active bleeding. Right image: bleeding ileal carcinoid. Case presentation: A 26-year-old otherwise healthy female presented with four episodes of rectal bleed- ing at home, initially described as hematochezia which evolved to appear more consistent with melena. Purpose: A 55-year-old white male presented with a four day history of nausea, vomiting, diarrhea and abdominal pain. The patient denied fever, chills, night sweats or unexplained weight loss. There was no history of melena or hematochezia. He denied recent travel or contact with individuals with similar symptoms. No previous surgeries. No family history of colon cancer or IBD. Vital signs: T102.2F, P117bpm, RR20br/min, and BP127/78. Abdominal exam revealed prominent distention, normoactive bowel sounds, and diffuse minor tenderness on deep palpation. No rebound or guarding. A tubular- shaped mass was palpated in the RLQ. Lab data: WBCs 1.5 x 103/uL with 35% bands. H/H, Plt, CMP, amylase, CEA, UA normal. Stool was Hemoccult positive. C. difficile toxin, fecal leukocytes, blood cul- tures, and toxicology were negative. Flat plate of the abdomen showed a mild high grade small bowel obstruction (SBO) without free air. CT revealed moderate to high-grade partial SBO with a transition point in the distal ileum. No evidence of free air or abscess. Exploratory laparotomy divulged small bowel largely dilated proximally with a large 6 x 5-cm Meckel’s diverticulum two feet from the ileocecal valve with no ischemia or necrosis. Adhesions from the Meckel’s tip to small bowel created a SBO that was resected. Pathology confirmed diagnosis. Meckel’s diverticulum is the most common congenital anomaly of the GI tract. It is usually clinically silent. If symptomatic in adults it generally presents as painless GI bleeding. Isolated cases have been reported in adults with SBO caused by adhesions from a Meckel’s diverticulum. Predisposition to develop symptoms is age less than 50, male sex, histologically abnormal tissue within the diverticulum and a diverticulum greater than two cm in length. As concluded in other case reports on SBO, there should be a high level of suspicion of Meckel’s preoperatively if there are no other obvious causes. Had we suspected this we could have ordered a Meckel’s scan, with a sensitivity of approximately 50%. Laparotomy can diagnose causation and lead to resection of Meckel’s diverticulum causing small bowel obstruction. Purpose: Video Capsule Endoscopy (VCE) and double balloon enteroscopy (DBE) are frequently uti- lized modalities to evaluate the small bowel in an elective outpatient setting. We present a case in which an actively bleeding carcinoid tumor was identified, treated for hemostasis, and localized with tattoo on an urgent, inpatient basis. This process assisted the surgeons in their pre-operative planning and inpa- tient management of the patient. Fg eT aT ORC WEL SRI CRR ESET Bes piers & PaaeCR! Pee: Dynes Fo PRT A ROR. BS EMeS RAP IEMONY date Bona eh FRY co Acie We: pe aED PaiAet xyeiemps Rat Ut Pas Urtiaee](https://figures.academia-assets.com/72315061/figure_170.jpg)
![[969] Meckel’s diverticulum.](https://figures.academia-assets.com/72315061/figure_171.jpg)

![[977] Large duodenal vrices with red wale sign in the second portion of the duodenum. Case report: A 71-year-old man with profound mental retardation was admitted with recurrent coffee- ground emesis. His care facility reported that his long-term PEG tube was functioning normally and it was confirmed to freely flush saline. There were no records available at their facility or at our institution regarding initial placement or subsequent replacements of the PEG tube. Examination showed a balloon- type replacement PEG tube that could be freely inserted and rotated, but only withdrawn to the 6-cm marking with traction. On review, a chest x-ray performed in the Emergency Department to confirm Discussion: Duodenal varices in the absence of cirrhosis are usually secondary to anomalies of the inferior vena cava, portal vein, splenic vein or superior mesenteric vein. Reported etiologies of vascu- lar associated varices include pancreatitis, surgical complications, congenital malformations, and crush injury. Interestingly, our patient recalled a crush injury secondary to motor vehicle accident (MVA) 40 years prior which necessitated exploratory laparotomy. Presumably, his mesenteric vein stenosis is a complication of the remote MVA. Due the paucity of cases, management is controversial. Endo- scopic injection sclerotherapy (ESL) is a promising modality; in our case 5% ethanolamine caused near complete resolution of his duodenal varices. Since the risk of bleeding is directly related to the size of the individual varix, routine surveillance and repeat ESL of high risk lesions could provide long term management of this condition, thus avoiding a risky surgical repair in an individual with multiple medical co-morbidities.](https://figures.academia-assets.com/72315061/figure_173.jpg)
![[979] Figure 1.](https://figures.academia-assets.com/72315061/figure_174.jpg)
![[980A] Axial CT scan image showing dilated small loops with bowel wall edema.](https://figures.academia-assets.com/72315061/figure_175.jpg)
![{980B] Coronal CT scan image showing dilated small loops with bowel wall edema.](https://figures.academia-assets.com/72315061/figure_176.jpg)


![[986A] Figure 3.Histopathology of mucinous cystadenoma showing intestinal type epithelium lining with large amount of apical mucin. Purpose: A routine colonoscopy on a 52-year-old female revealed an enlarged appendix with a wide base prolapsing into the cecum. CT-abdomen revealed a 3.0 x 1.2-cm uniform hypodense “mucocele” involv- ing the appendix. As the lesion involved the base of the appendix and prolapsed into the cecum, laparo- scopic hemicolectomy for resection was performed. Histopathology revealed a mucinous cystadenoma of the appendix with no dysplasia. A detailed intra-operative exploration of the gastrointestinal tract, ovaries and peritoneum for coexisting malignancies was negative. Follow-up colonoscopies and pelvic exams were unremarkable. Here, we report successful resection of a low-grade appendiceal mucinous neoplasm by laparoscopic right hemicolectomy, strengthening the evolving consensus that laparoscopic approach is safe and feasible and a hemicolectomy can allow safer laparoscopic resection by avoiding direct handling of tumors.](https://figures.academia-assets.com/72315061/figure_179.jpg)
![[986B] Figure 1. Colonoscopic view of cecum showing base of the appendix prolapsing into the cecal lumen.](https://figures.academia-assets.com/72315061/figure_180.jpg)
![[986C] Figure 2. CT scan of the abdomen and pelvis showing mucocele.](https://figures.academia-assets.com/72315061/figure_181.jpg)

![[989] Arrow indicates “hooked” appearance of celiac artery due to compression by medial arcuate ligament from above. Discussion: Patient with chronic abdominal pain associated with weight loss and exacerbations with exercise should have MALS in the differential. Eating stimulates increased metabolic demand for the stomach leading to mismatched perfusion via a compromised celiac artery. During exercise, the dia- phragm expands at a higher frequency and force to accommodate for increased oxygen demand. This leads to further reduction of celiac artery flow in patient with MALS. CT Sagital images demonstrating acute angulation and narrowing of the proximal celiac artery causing a “hooked” appearance (arrow) is characteristic of median arcuate ligament syndrome.](https://figures.academia-assets.com/72315061/figure_183.jpg)

![[995] EGD: periampullary diverticular ulcer.](https://figures.academia-assets.com/72315061/figure_185.jpg)
![[998B] Figure 2. Image demonstrates narrowing of the distance between the SMA (arrow) and the aorta (A) at the level of the 3rd portion of the duodenum (arrowhead). [998A] Figure 1. Axial contrast CT image obtained during the portal venous phase demonstrates a non-occlusive thrombus within the right portal vein (arrow).](https://figures.academia-assets.com/72315061/figure_186.jpg)


![Purpose: Duodenal diverticular bleeding is an uncommon cause of upper GI bleeding where endoscopic hemostasis in patients with ongoing need of antiplatelet agents poses a diagnostic and therapeutic chal- lenge. We present a rare case of periampullary duodenal diverticular bleeding in a patient receiving dual antiplatelet therapy. An 80-year-old female presented with dizziness, diaphoresis and melena. Her signifi- cant past history included coronary disease with recent stents on dual anti-platelet agents. On admission, she was found to be anemic (Hb 6 g/dL) requiring blood transfusions for hemodynamic stabilization. EGD showed two large periampullary diverticuli in the duodenum (Figure 1) with a slow active oozing on one of the diverticular folds with underlying visible vessel. Two hemoclips were applied to achieve hemostasis. Area up to mid-jejunum showed other small non-bleeding, duodenal and jejunal diverticuli. After volume resuscitation, patient recovered uneventfully and discharged home on PPI and aspirin. She was readmitted three days later with anemia and melena, requiring blood transfusion. Aspirin was held and she was discharged home on a single antiplatelet agent. Incidence of duodenal diverticular bleeding in patients on dual antiplatelet therapy is not currently known. A meta-analysis from 50 clinical trials showed higher rate of GI bleeding associated with aspirin at doses >325 mg/d; 2.5% (95% confidence interval [CI] 1.8-3.1%) A recent pooled analysis report the incidence of major bleeding necessitating hospitalization to be 1% in patients on 325 mg/d or less of aspirin alone, 0.85% with clopidogrel alone, and 1.7% with aspirin plus clopidogrel. The prevalence of duodenal diverticuli has been described to be from 0.06-22%; however, given its infrequency, the incidence of bleeding and impact of antiplatelet therapy remains unclear. Our case illustrates a potential higher bleeding risk due to dual-antiplatelet therapy in patients with duodenal diverticuli. It is imperative for the endoscopist to be cognizant of this rare complication to be able to recognize and institute appropriate endoscopic therapy.](https://figures.academia-assets.com/72315061/figure_189.jpg)

![[1008] Left image: Severe duodenitis caused by WG. Right image: Multiple duodenal ulcers caused by CMV. Purpose: A 55-year-old male presented with arthralgias, fevers, cough, abdominal pain, and melena. Initial evaluation demonstrated elevated ESR and CRP, eosinophilia, hematuria, and proteinuria. Abdominal CT revealed duodenitis, following by EGD with ulcerated duodenitis. Biopsies had increased eosinophils and submucosal hemorrhage. A biopsy of palpable purpura of the feet suggested vasculitis. C-ANCA was positive with an elevated proteinase-3 antibody. This constellation was diagnostic of Wegener's granulomatosis (WG). Symptoms improved with high-dose IV corticosteroids and he was transitioned to oral prednisone at discharge. His WG relapsed and he was treated with rituximab. His course was complicated by C. difficile-associated diarrhea which responded to metronidazole. Three days after the last infusion of rituximab, he returned with severe C. difficile colitis requiring colectomy with end-ileostomy. Despite antibiotic therapy after surgery, he had persistent high ileostomy output and anemia. Repeat endoscopy showed severe ulcerated duodenitis, despite the absence of other systemic or cutaneous vasculitis. Several ulcers were successfully treated endoscopically. Several hours later the patient became unstable with a duodenal perforation requiring surgery. Further complications followed, including bacteremia, fungemia, and sepsis. Ongoing GI bleeding not amenable to endoscopic therapy required more transfusions and surgical intervention. Results of serum serologies and the second duo- denal biopsies eventually proved cytomegalovirus (CMV) duodenitis. Antiviral therapy was added to his other therapies, but ongoing sepsis, bleeding, and pulmonary failure resulted in the patient’s demise less than three months from his initial presentation. WG is a systemic disease characterized by necrotiz- ing granulomatous inflammation and small- to medium-sized vasculitis in multiple organs. Commonly involving the respiratory tract and kidneys, GI tract involvement is rare. WG treatment requires immu- nosuppression, risking development of opportunistic infections. A high degree of suspicion for CMV is needed to identify immunocompromised patients that may benefit from empiric therapy during severe illness. Endoscopy carries a high risk of perforation in this setting. Purpose: Bariatric surgery is a highly effective treatment for morbid obesity and its associated conditions. Meanwhile, surgery in obese patients is associated with worse outcomes than in non-obese patients. In this report, we describe our first experience with a two-stage procedure for a morbidly obese patient with type 2 diabetes mellitus (T2DM) and a nonfunctioning pancreatic neuroendocrine tumor (PNET). A morbidly obese, 63-year-old woman presented to our unit for the evaluation of a pancreaticoduode- nectomy (PPPD) to treat a pancreatic tumor. Her body mass index (BMI) was 40.0 kg/m2. Computed tomography revealed a 30-mm tumor in the pancreatic head, and she was diagnosed with PNET. She had several obesity-related diseases, including T2DM. She had received insulin treatment for 6months. Because PPPD is highly risky in morbidly obese patients, we planned a two-stage surgery—laparoscopic sleeve gastrectomy (LSG) followed by laparoscopic-assisted PPPD. First, LSG for morbid obesity was performed. The length of the postoperative hospital stay was 5 days, with no morbidity. Six month after LSG, her BMI had decreased from 40.0 to 29.3 kg/m2. Ghrelin levels before the operation and 2 weeks, 1 month, and 6 months after the operation were 129, 21, 28, and 25 fmol/ml, respectively. The patient also experienced complete remission of her T2DM without medication 2 weeks after LSG. Seven months after LSG, laparoscopic-assisted PPPD was performed. The length of the postoperative hospital stay was 23 days, with no morbidity. Glucagon-like peptide 1 (GLP-1) levels increased (Figure) and glucose- dependent insulinotropic peptide (GIP) levels decreased after PPPD. In conclusion, we have reported an important case in which two-stage surgery comprising laparoscopic-assisted PPPD, after LSG, was per- formed in a morbidly obese patient. The findings in this case suggest that two-stage surgery may be useful for decreasing postoperative complications and can help explain the changes in glucose metabolism. It is suggested that the post -prandial changes of ghrelin and GLP-1 levels lead to be complete remission of T2DM, whereas pancreatic resection is considered a risk factor for diabetes due to insulin deficiency.](https://figures.academia-assets.com/72315061/figure_191.jpg)


![[1015A] Figure 1. Discussion: Splenic artery embolization has not been studied well in cases of SRS secondary to IM. The majority of the literature is on splenectomy in unstable patients or non-operative watchfulness in stable patients. This methodology preserves spleen and prevents the dreadful complication of over- whelming post splenectomy infection, risks of laparotomy and the consequent morbidity and mortality in apslenic patients.](https://figures.academia-assets.com/72315061/figure_194.jpg)

![[1019] Low-grade follicular B cell lymphoma, jejunum. 1021](https://figures.academia-assets.com/72315061/figure_196.jpg)


![[1026] Case descriptions with endoscopic and histopathological findings](https://figures.academia-assets.com/72315061/table_007.jpg)


![{1031] Abdominal CT scan demonstrating small bowel intussusception. Purpose: A 47-year-old lady presented to the emergency room with abdominal pain associated with vom- iting and non-bloody diarrhea for 2 days. She was hemodynamically stable and her physical examination was unremarkable. A contrast-enhanced CT scan of the abdomen revealed numerous dilated fluid-filled small bowel loops with a small bowel intussusception in the right lower quadrant (Figure 1). She subse- quently underwent an exploratory laparotomy which showed a severely dilated bowel with a large segment of intussusception. On the proximal portion of the intussusception, there was a 3-cm intraluminal mass as well as large 5-cm mass at the distal end of the intussusception. There was an additional non-obstructing 2-cm mass in the distal small bowel. Frozen section of the mass was suggestive of malignant melanoma. The intussuscepted bowel was resected and a side-to-side anastomosis was performed. There was no other evidence of metastatic disease in the abdomen. The diagnosis of BRAF-positive small bowel melanoma was confirmed on subsequent examination of the resected specimen. The resected margins were tumor free and 3 out of 15 resected lymph nodes were involved by tumor spread. A detailed skin survey did not reveal any suspicious lesions to account for a primary site. Melanoma of the small intestine in the absence of an obvious skin lesion is a rare tumor and an unusual cause of intussusception in adults. In a large cohort of 84,836 cases of melanoma, approximately 2% had an unknown primary site. Whether primary small bowel melanoma is a separate entity is a matter of ongoing debate. Some authorities believe that all small bowel melanomas are metastatic from unknown or regressed primary cutaneous melanoma. The presence of a solitary lesion, the lack of distant metastasis, and a long disease-free survival after bowel resection all favor a diagnosis of primary small bowel melanoma. The small bowel is a common site for metastatic melanoma and these patients have a better prognosis compared to those with primary bowel melanoma. Management is aimed at wide local resection and adjuvant chemotherapy with close surveillance.](https://figures.academia-assets.com/72315061/figure_201.jpg)
![[1033] Cholecystectomy clip in duodenum. Purpose: Laparoscopic cholecystectomy with use of metallic surgical clips is a safe procedure with a less than 3% overall complication rate. We are reporting a rare case of migrated cholecystectomy clips into the duodenum associated with postbulbar stricture and ulcer. 68 year old female with history of cholecys- tectomy, metastatic colon cancer treated with right hemicolectomy, chemotherapy, and radiofrequency ablation of liver lesions. She was disease free for 5 years until a new right hepatic lobe lesion was discov- ered and treated with stereotactic radiation therapy with incomplete success. A year later, she presented with obstructive jaundice from malignant biliary stricture which was treated with a metal stent. Recently, she presented with acute cholangitis and gastric outlet obstruction. EGD showed an intrinsic postbulbar duodenal stricture requiring balloon dilation to 15 mm. There were no complications post dilation and cholangitis was treated with stenting. Progressive duodenal stricture lead to repeat endoscopic evaluation showing the postbulbar stricture and a deep ulcer with metallic clips seen at the ulcer base. Simultaneous fluoroscopic imaging confirmed that these were cystic duct clips eroding into the duodenum. This was also confirmed with CT scan. Many clip-associated complications, such as biliary leaks, clip migration into the common bile duct, and clip embolism have been reported. Migration of endo-surgical clips into the duodenum is a rare complication, previously reported in only five cases. In all the reported cases, an ulcer was present as in our case. Additionally, the ulcer was large and bleeding, and endoscopic or surgical treatment was required. Our case is the first report of migrated cholecystectomy clips into the duodenum to be associated with stricture and previous radiation. Proposed mechnisms: 1. the base of the](https://figures.academia-assets.com/72315061/figure_202.jpg)

![ee eae ee nee ee ee N NNE EEE EEN SOE PD IOI IIS DLE OIE NE ONO Raji Shameem, MD, Niket Sonpal, MD, Benyam Alemu, MD, Ladan Ahmadi, MD. Lenox Hill Hospital, Dix Hills, NY. [1035A] Stomach biopsy.](https://figures.academia-assets.com/72315061/figure_204.jpg)

![1040 [1038B] Images showing petechial hemorrhaging of small bowel with no ischemia.](https://figures.academia-assets.com/72315061/figure_206.jpg)
![[1038A] Small bowel circumferential wall thickening and edema.](https://figures.academia-assets.com/72315061/figure_207.jpg)

![{1041] Image 1. Retroperitoneal mass on endoscopic ultrasound.](https://figures.academia-assets.com/72315061/figure_209.jpg)


![[1050] Figure 1. CT of the patient's spine showing metastases (arrow is pointing to T10).](https://figures.academia-assets.com/72315061/figure_211.jpg)





![Introduction: Hepatogastric fistulalHGF) is a rare but serious complication of Transcatheter arterial embolization [TAE ] of hepatic artery for hepatocellular carcinoma. We present a case of](https://figures.academia-assets.com/72315061/figure_217.jpg)
![[1073] Table 1. Laboratory findings Purpose: A 36-year-old Caucasian male without prior medical history initially presented to another facility with one week of right upper quadrant (RUQ) abdominal pain, jaundice and fatigue. After abnor- mal lab values (Table 1) were found, he left that facility and presented to this hospital. He admitted to weekend binge drinking and drank 10 beers three hours prior to symptom onset. He denied taking herbal remedies, homeopathic medications or other supplements. He drank up to three energy drinks (Figure 1) on a daily basis for the past year. Physical exam showed stable vital signs, jaundice, spider nevi and RUQ tenderness. Initial work-up was negative for viral, ischemic or autoimmune hepatitis. On HD #6,](https://figures.academia-assets.com/72315061/table_009.jpg)
![[1070] Liver biopsy showing portal inflammation with bile duct injury, pericholangitis, and kupffer cell and histiocyte hypertrophy with occasional erythrophagocytosis.](https://figures.academia-assets.com/72315061/figure_218.jpg)




![{1076] Bladder varices on CT abdomen/pelvis (red arrow). Discussion: This case demonstrates an uncommon etiology of symptomatic anemia and gross hematuria from urinary bladder varices due to portal hypertension. Indeed, reports of bleeding bladder varices appear in only a handful of cases in the literature. Ectopic varices are portosystemic shunts that can occur anywhere in the GI tract. Intra-abdominal surgery with subsequent adhesions can impede the normal port-systemic anatomy, forming unusual collateral routes. This is the purported mechanism of bladder variceal formation, which is consistent with the patient’s history of appendectomy. Treatment of ectopic varices depends on the clinical scenario, but can range from variceal embolization to beta blockade. With a patent portal vein, TIPS can successfully control bleeding via portal decompression, as was performed in this case. In any patient with portal hypertension, it is important to consider the possibility of ectopic varices in the presence of unexplained visceral bleeding.](https://figures.academia-assets.com/72315061/figure_222.jpg)



![{1085] Figure 1. A) CT Abdomen with mass in the RLQ. B) Polygonal crystals with “fish scale” appearance.](https://figures.academia-assets.com/72315061/figure_225.jpg)
![[1091] Table 1. Laboratory data on hospital admission One Train Can Hide Another: Ascites in a Cirrhotic Patient Kawtar Alkhalloufi, MD, Juan Blum Guzman, MD, Edula Raja, MD, Zahid Vahora, MD, Hicham Khallafi, MD, Kamran Qureshi, MD. Florida Hospital, Orlando, FL. Purpose: Although there are several reported cases of niacin-induced hepatotoxicity, niacin-induced cholestatic hepatitis (CH) is very rarely reported in the medical literature. We report a case of niacin- induced CH in a patient with liver cirrhosis. A 61-year-old man with CAD, hyperlipidemia, prostate cancer and status-post prostatectomy was referred for abnormal liver function tests (LFTs). He had thrombocytopenia, which was incidentally found during the preoperative work-up of an elective her- nia repair. Home medications included omeprazole, aspirin, clopidogrel, metoprolol and niacin. He wa: taking niacin-SR 2 gm daily for approximately 6 months. He denied history of alcohol abuse. Physical examination was remarkable for jaundice, ascites and mild pitting edema of legs. Lab data is shown in the table. Patient was admitted to the hospital for further work-up of the progressively worsening LFTs. Niacin was held for severe hepatitis. MRI of the abdomen showed small nodular liver, moderate ascites and a distended gallbladder with multiple gall stones. HBsAg, Hep C antibody and Hep A IgM anti- body were non-reactive. Serological work up for hemochromatosis (including gene mutation analysis). autoimmune hepatitis and Wilson's disease were negative. Tumor markers including serum alpha-fetc protein, serum carcinoembryogenic antigen and serum prostate specific antigen levels were non-signifi- cant. Liver biopsy showed moderate-severe chronic active hepatitis, bridging fibrosis without evidence of malignancy. Liver enzymes gradually trended down with conservative management after stopping niacin. Niacin was not initially suspected as the cause of this decompensation due to the primary cho- lestatic profile. However, it was later attributed to niacin as he developed CH during treatment with the drug; he improved immediately after stopping the drug, while other potential causes were ruled out. Tc our knowledge, there is only one reported case of niacin-induced CH (Patel SD et al., 1994). Clinicians should be aware of this rare association of niacin with CH; cirrhotic patients may be more vulnerable.](https://figures.academia-assets.com/72315061/table_012.jpg)

![{1103] Arrow indicates gallstone within an intrahepatic abscess. with conservative therapy, and emergent transplant was not necessary. Direct evidence for suppressive antibiotic therapy does not exist, but given the uneven, porous surface of gallstones and the experience with retained renal stones, it is reasonable to continue antibiotics in such cases.](https://figures.academia-assets.com/72315061/figure_227.jpg)
![[1106] H &E staining of liver biopsy showing accumulation of glycogen in hepatocytes.](https://figures.academia-assets.com/72315061/figure_228.jpg)
![{1116A] Figure 1. Histology reveals cholestatic hepatic tissue with a subtle infiltration by deeply pigmented, hepatoid cells which clearly mark as melanocytes. there have only been a few cases reported in the literature with metastatic melanoma of unknown origin initially presenting as fulminant hepatic failure.](https://figures.academia-assets.com/72315061/figure_229.jpg)



![{1122] Figure 1. CT abdomen with contrast showing cirrhotic liver with heteroge- neously enhancing 3.1cm ruptured lesion within the caudate lobe with hematoma of the lesser sac. Discussion: Spontaneous rupture of HCC is associated with a high inpatient mortality of 25-75%. Hema- toma of lesser sac as a consequence of a ruptured HCC with hemoperitoneum is a relatively rare presen- tation. Surgical resection of tumor is associated with higher risk of complications, especially in patient: with concomitant cirrhosis. Radiofrequency ablation is technically difficult, due to the deep location o: the tumor. TACE is the preferred loco-regional approach for tumor in caudate lobe, with good rate o: success in controlling bleeding.](https://figures.academia-assets.com/72315061/figure_233.jpg)
![{1131] Figure 1. Liver histology, hematoxylin and eosin stain. A. Infiltration of a portal tract with predominantly eosinophils. B. High power view demonstrating ballooning changé and eosinophilic infiltrate. C. Submassive hepatic necrosis. D. High power view of adjacent preserved liver with eosinophilic infiltrate. Introduction: Clinicians have become increasingly reliant on imaging studies to make diagnoses. Despit improved sensitivity of these imaging modalities, some diagnoses cannot be made without biopsy Purpose: Data on the adverse event profiles of the incretin-based hypoglycemic agents are limited. We present the first case of drug-induced liver injury (DILI) secondary to the glucagon-like peptide 1 (GLP-1) agonist liraglutide. Case: A 29-year-old woman with type 2 diabetes and vitiligo presented with 10 days of nausea, emesis, and acnte henattic Other than starting lirachitide 1:7 mo daily faur manthe nrine the nathient rennrted no](https://figures.academia-assets.com/72315061/figure_234.jpg)






![{1154B] MRCP: enhanced ill-defined liver mass.](https://figures.academia-assets.com/72315061/figure_241.jpg)
![{1154A] CT scan: intrahepatic biliary dilation, no hilar mass. Discussion: Cholangiocarcinoma, histologically classified as adenocarcinoma, appears as bile duct thickening or biliary dilation on CT scan. On MRI, malignant tissue appears hypointense, as compared to liver parenchyma on T1 images and hyperintense on T2 images.](https://figures.academia-assets.com/72315061/figure_242.jpg)


![[1173A] Figure 1. Coronary angiogram showing normal coronary arteries.](https://figures.academia-assets.com/72315061/figure_245.jpg)
![[1173B] Figure 2. T2 weighted MRI of bilateral hips showing area of enhancemen' showing avascular necrosis of left hip.](https://figures.academia-assets.com/72315061/figure_246.jpg)
![{1180] Thorotrast-induced enhancement of spleen. Ascites also present. Purpose: We present the case of an 83-year-old female who presented with recurrent ascites and chronic liver disease of uncertain etiology. Paracentesis revealed fluid with a SAAG >1.1, suggestive of portal hypertension. Liver work-up, including autoimmune labs, viral hepatitis serologies, and iron studies, were unremarkable. Additional lab work was significant for thrombocytopenia and a normal CEA. Medical history was negative for alcohol abuse, diabetes, and obesity. Liver ultrasound with Doppler was normal, with no evidence of thrombosis, focal intrahepatic abnormalities, or biliary duct dilatation. CT of the abdomen with contrast demonstrated a cirrhotic-appearing liver along with prominent, con- trast-enhancing high density material within the spleen and peripancreatic lymph nodes. Transjugular liver biopsy demonstrated periportal fibrosis, along with focal granular foreign body material. Upon further inquiry, it was elucidated that the patient had received Thorotrast for imaging of a cirosoidal aneurysm in the 1950s. Thorotrast, a radioactive suspension containing thorium dioxide, was used as a contrast agent in the United States up until the late 1950s. Thorotrast offered high image quality and, at that time, no immediate side effects were noted. As was the case in our patient, it was primarly used for cerebral angiography. Worldwide, approximately 100,000 people were exposed to Thorotrast from 1930 to 1964. Subsequently, it was discovered that Thorotrast induced liver disease and tumors decades after its use. Our case is unique in that Thorotrast-induced chronic liver disease is seldom seen in modern-day clinical practice.](https://figures.academia-assets.com/72315061/figure_247.jpg)

![[1183] Direct portal venography during TIPS demonstrates hepatofugal flow in the SMV with a dense network of duodenal varices (arrow). PV-portal vein, GV-gonadal vein. Conclusion: Portosystemic shunting can occur in unusual locations, leading to atypical location of varices and hemorrhaging in the cirrhotic with high morbidity and mortality, if not quickly identified. While no guidelines exist on management of these varices, treatment ultimately requires a multidisci- plinary approach.](https://figures.academia-assets.com/72315061/figure_249.jpg)
![[1188A] Incomplete septal fibrosis. requiring transplantation. Liver biopsy remains the gold standard in diagnosing NCPH and in identify: ing typical vascular and architectural changes of NCPH.](https://figures.academia-assets.com/72315061/figure_250.jpg)
![[1188B] Portal vein ectasia.](https://figures.academia-assets.com/72315061/figure_251.jpg)
![[1198] Table 1. Peritoneal cultures with intraperitoneal and intravenous antibiotic therapy 1200](https://figures.academia-assets.com/72315061/table_013.jpg)


![[1209A] Endoscopic view of toothpick embedded in antrum. Purpose: A 46-year-old male presented on an outpatient basis for upper gastrointestinal endoscopy and endoscopic ultrasound after being diagnosed with elevated liver enzymes, unexplained weight loss, and a mildly dilated pancreatic duct on an outpatient CT of the abdomen and pelvis. His liver function tests were unavailable to us at the time, but pre-procedural labs showed an AST of 71 U/L (high normal 59) and an ALT of 115 U/L (high normal 72), with normal total bilirubin and alkaline phosphatase. Dur- ing upper gastrointestinal endoscopy, a wooden object was seen embedded into the medial aspect of the antrum, thought to be a toothpick. Endoscopic ultrasound revealed a sharp tip to the object with its tip exiting the stomach and invading the liver. Laparoscopic surgery was performed which clearly showed the sharp end of a toothpick penetrating the liver, and upon removal, the liver bed began to bleed profusely, which was stopped using Surgicel. The antral perforation was also sealed using Evicel. Upon further questioning during the workup, the patient did remember accidentally swallowing a toothpick a few weeks prior. Of note, there were no other abnormalities on endoscopic ultrasound other than the presence of the toothpick.](https://figures.academia-assets.com/72315061/figure_254.jpg)

![{1209B] Endoscopic ultrasound showing toothpick penetrating the liver.](https://figures.academia-assets.com/72315061/figure_255.jpg)
![[1209C] Laparoscopic view of toothpick exiting stomach with laparoscopic forcep covering the liver puncture site. An Unusual Cystic Mass of the Liver 1210](https://figures.academia-assets.com/72315061/figure_256.jpg)
![{1210] Different treatment time points and changes to tacrolimus dose. [1210] Laboratory tests and virological responses](https://figures.academia-assets.com/72315061/figure_257.jpg)
![[1214] Primary hepatic leiomyosarcoma: 32 x 23 x 13.5 cm specimen. mass in the epigastric area, and +3 lower extremity edema. He had anemia (9.9 g/dL) and abnormal liver function tests. Radiologic imaging revealed a 17-cm complex mass in the right lobe of the liver. A liver biopsy was performed. Immunohistochemistry revealed tumor cells reactive for smooth muscle actin and desmin, which was consistent with high-grade leiomyosarcoma. He underwent right hepatic lobec- tomy via a thoracoabdominal approach. A 32 x 23 x 13.5 cm hemihepatectomy specimen was resected with portions of adherent diaphragm, leaving the diaphragmatic margin free of involvement. The patient subsequently received chemotherapy with Ifosfamide and mesna for residual tumor, which was well tol- erated. The patient is doing relatively well 24 months after tumor resection, with no recurrence to date. This rare case of PHL is one of 30 cases reported in the English literature. Prognosis is influenced by the ability to resect the tumor completely. Liver transplantation (OLT) in such patients was accompanied by early high recurrence with poor outcomes after 1 year. In our patient, a good outcome was obtained with resection and chemotherapy, despite having advanced disease. International multi-registry efforts need to be established to assess the most effective therapeutic modalities for PHL.](https://figures.academia-assets.com/72315061/figure_258.jpg)
![{1219A] Thickening in the ascending colon. Discussion: S. Mississippi makes up 0.9% of U.S. Salmonella infections, typically limited to the Eastern US. S. Mississippi is commonly reported in Tasmania, Australia, with an annual rate of 17/100,000 peo- ple. Indirect contact with native birds, untreated drinking water and travel within the state are predictors for the disease. On average, the illness lasts for 6 days and 68% of those infected experience >11 bouts of diarrhea per day. No reports of colonic masses with salmonellosis exist. Investigation is needed to deter- mine whether a colonic mass is a possible manifestation specific to S. Mississippi or if it is an incidental finding overlooked in many Salmonella infections.](https://figures.academia-assets.com/72315061/figure_259.jpg)
![[1219B] Mass in the ascending colon.](https://figures.academia-assets.com/72315061/figure_260.jpg)
![[1220] CT of the abdomen and pelvis showed an IUD (red arrow) and a 4.7 x 1.4.cm hypodensity with fluid attenuation (blue arrow). —————— Case Report: A 50-year-old woman presented for a routine colonoscopy to screen for colon cancer. She had not disclosed a medical history of menstrual cramping and menometrorrhagia, for which an intra- uterine device (IUD) was placed two years prior. Colonoscopy revealed a sessile tubular adenoma in the ascending colon, which was removed via cold biopsy forceps. Three hours post-colonoscopy, she devel- oped lower abdominal pain that progressed to fevers. Upon presentation to the emergency department, a physical exam revealed vaginal discharge, cervical motion tenderness, and left adnexal tenderness. Computed tomography (CT) of the abdomen and pelvis showed a 4.7 x 1.4-cm left adnexal hydrosalpinx and a displaced IUD, suggestive of pelvic inflammatory disease. After 3 days of inpatient treatment with intravenous antibiotics, she was discharged home on oral antibiotics and had an unremarkable recovery. Discussion: We present a TOA exacerbation as a possible cause of acute pelvis after colonoscopy. Although impossible to prove, the likely culprit was traction on the pelvic organs by colonoscopic manipulation, which may have resulted in direct trauma or irritation of the TOA and IUD. Gynecologic pathologies are infrequently discussed as a cause for post-colonoscopy pain, but there are prior reports of post-colonoscopy complications associated with endometriosis, pelvic actinomycosis, ovarian malig- nancies and TOAs. Awareness of these rare, but potentially serious, complications may lead to earlier wrornntnitinn and awnidanca nl lifes therantanina cannalasa](https://figures.academia-assets.com/72315061/figure_261.jpg)
![[1224] Figure 1. Sigmoidoscopic view of solitary rectal ulcer. Conclusion: SRUS must be borne in mind when patients present with symptoms of a defecatory disor- der and hematochezia, in association with rectal ulceration (with associated typical histologic findings). Conservative medical therapy may improve symptoms, reserving biofeedback, and surgical intervention for more refractory cases.](https://figures.academia-assets.com/72315061/figure_262.jpg)
![[1226A] Figure 1. Retroflexed view of polypoid distal rectal mass.](https://figures.academia-assets.com/72315061/figure_263.jpg)

![{1226B] Figure 2. Anterograde view of mid rectal polypoid masses.](https://figures.academia-assets.com/72315061/figure_265.jpg)
![Discussion: Rectal syphilis is rare and can be misdiagnosed or missed due to absence of symptoms. Clinically, patients may present with anorectal pain, tenesmus, bleeding, itching, or anal discharge. Endo- scopically, rectal syphilis can appear as a destructive rubbery lesion with single or multiple ulcers. The combination of clinical and endoscopic features mimic other anorectal pathologies, such as rectal cancer. inflammatory bowel disease (ulcerative proctitis), solitary rectal ulcer, or viral anorectal ulcers (herpes simplex virus, gonorrhea, Chlamydia, and lymphogranuloma venereum). Tissue biopsy is recommended for diagnosis with dark-field microscopy or PCR. A detailed sexual history is important, and evalua- tion for other sexually transmitted infections should be performed. Once diagnosed, patients should be treated with intramuscular benzathine penicillin (or doxycycline in those with a penicillin allergy). Ou patient received intramuscular benzathine penicillin G, 2.4 million units weekly for 3 weeks and had complete resolution of his symptoms. [1228] Colonoscopy: rectal lesion.](https://figures.academia-assets.com/72315061/figure_266.jpg)





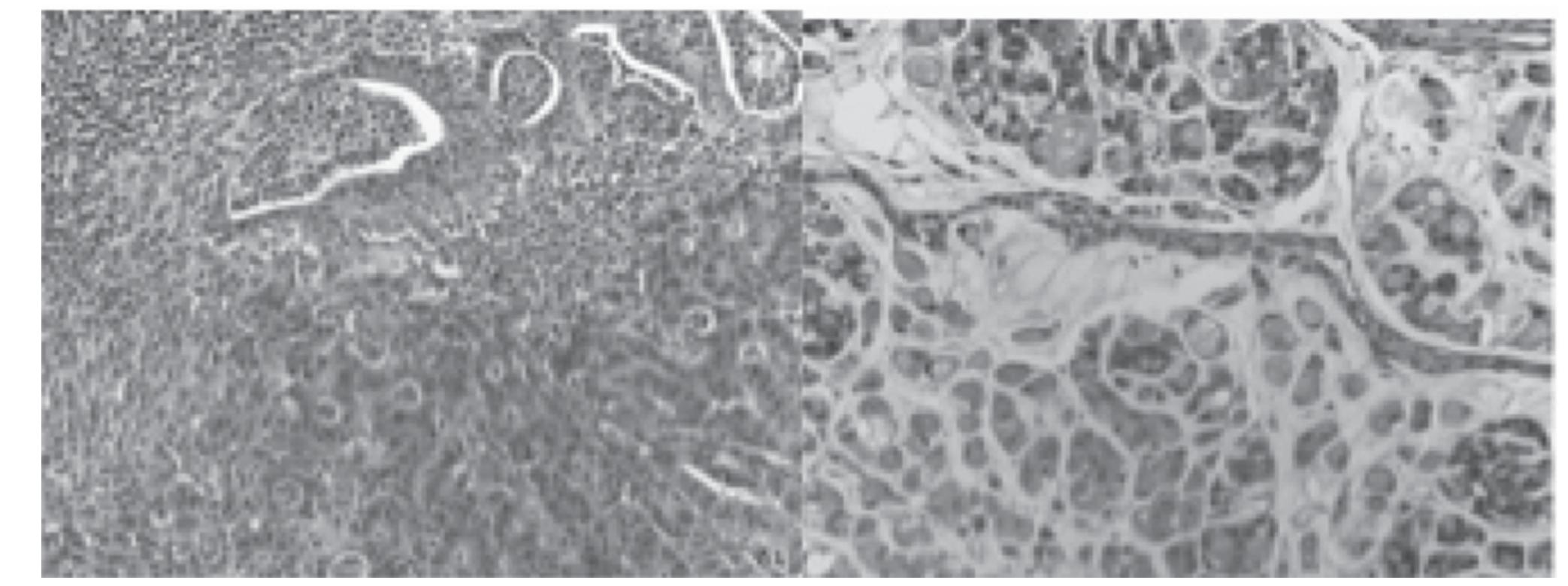


![[1243B] CT scan: mesenteric lymphadenopathy. Purpose: Gastrointestinal tract lymphomas, although rare, account for about 1% of all colorectal malig- nancies, and colorectal lymphomas account for about 10-20% of all GI lymphomas. We present an atypi- cal case of primary colonic lymphoma incidentally diagnosed on colonoscopy. A 70-year-old man with hypertension and peptic ulcer disease presented with constipation and blood-streaked stools. He denied weight loss, fevers or night sweats. His physical exam was negative for abdominal or pelvic masses and lymphadenopathy. Three years prior, he had a colonoscopy that showed only one reactive non-dysplastic 4-mm ascending colon polyp that was completely resected and retrieved. On repeat colonoscopy, there were multiple patchy areas of circumferential friability, edema and erythema in the colon, most notable in the ileocecal valve (Image 1). Multiple biopsies confirmed diffuse follicular B-cell lymphoma, which was CD-20 positive. Subsequent laboratory tests, including CBC, LDH and B2- microglobulin were nor- mal. Abdominal CT revealed right-sided mesenteric lymphadenopathy suspicious for nodal metastasis (Image 2). A bone marrow aspirate and trephine showed no evidence of bone marrow involvement. The patient was diagnosed with stage IIAE follicular lymphoma on the modified Anne Arbor classification, and was initiated on bendamustine- rituximab chemotherapy. According to Rummel et al, this regimen Case: A 76-year-old white male was initially admitted with a 1-month history of chronic diarrhea, with a negative CDI toxin at an outside hospital. A colonoscopy showed severe pan-colitis with pseudomem- branes, and a subsequent CDI toxin was positive. The colonoscopy was complicated by perforation of the right colon, which required a right hemicolectomy with primary anastomosis (30 cm resected) and](https://figures.academia-assets.com/72315061/figure_275.jpg)
![[1242] Sigmoid colon. of metastasis include the lung, liver, bone and brain. Metastasis to the colon is rare. The detection o! metastatic IDC detected in colonoscopy is even more rare. This case underscores another anecdotal ben- efit of screening colonoscopy in a patient with prior non-gastrointestinal malignancy.](https://figures.academia-assets.com/72315061/figure_276.jpg)
![{1243A] Colonoscopy: ileocecal valve. resulted in increased progression-free survival and harbored fewer toxic side effects than R-CHOP in patients with indolent colonic lymphoma. In conclusion, although patients with primary colonic lym- phoma usually present with symptoms of abdominal pathology including pain, weight loss or a palpable abdominal mass, our patient only had indolent signs of disease. Therefore, this diagnosis requires a high index of clinical suspicion. Our case also highlights the importance for repeat colonoscopy and further investigation in patients with vague gastrointestinal symptoms.](https://figures.academia-assets.com/72315061/figure_277.jpg)
![{1247B] Ulcerated mass with surrounding erythema. [1247A] Lesion in the colon causing partial obstruction.](https://figures.academia-assets.com/72315061/figure_278.jpg)

![[1248] CT Chest showing pneumomediastinum. Discussion: Incidence of colon perforation is common with therapeutic, as compared to diagnostic, colo- noscopy. Subdiaphragmatic free air suggest intraperitoneal perforation, whereas subcutaneous emphysema, pneumoretroperitoneum, and pneumomediatinum suggest extraperitoneal perforation. Extraperitoneal perforation without peritoneal signs can be treated conservatively with bowel rest and antibiotics. Micro- perforation usually close with omental adherence, and symptoms resolve within 24-48 hours.](https://figures.academia-assets.com/72315061/figure_280.jpg)
![[1249] Chronic granulomatous colitis post pneumatic balloon dilation. Our case is unique in the chronicity of active inflammation, as well as the presence of foreign body granu- lomata. Coffee enemas have been gaining in popularity, most commonly cited for constipation relief and as a method of “detoxification.” This case highlights the potential harm associated with this unproven therapy. Animal models may help better understand what component of coffee may be responsible for inducing a chronic foreign body granulomatous transmural colitis.](https://figures.academia-assets.com/72315061/figure_281.jpg)




![[1256] Hematoxylin and Eosin stain. Discussion: Leiomyomas are benign, smooth muscle tumors and are rarely found in the gastrointestinal tract, with only 3% in the colon. Colonic leiomyomas are mostly found incidentally, and can occur in the sigmoid and transverse colon, and less commonly in the rectum. Most cases are usually asymptomatic and seen in the third decade of life, with a slight female predominance. They arise from the muscularis mucosa, muscularis propria or from vascular smooth muscle. Endoscopically, they present as intramural or pedunculated growths, appearing similar to adenomatous polyps. Immunostain is positive for actin and desmin, and negative for CD34 and CD117 (C-kit), which helps to differentiate them from GISTs. Snare polypectomy is adequate, but for larger tumors or when malignancy is a concern, surgical resection with wide margins is recommended.](https://figures.academia-assets.com/72315061/figure_286.jpg)





![[1264A] Figure A. Normal appendiceal orifice and cecum at initial colonoscopy.](https://figures.academia-assets.com/72315061/figure_292.jpg)
![[1264B] Figure B. Polypoid lesion noted in the cecum at repeat colonoscopy.](https://figures.academia-assets.com/72315061/figure_293.jpg)
![[1266] Figure 1. A) Circumferential Malignant-Appearing Mass in the sigmoid colon. B) Biopsy of mass depicting ulcerative changes with abundant plasma cells. Staining showing C) Lambda protein and D) Kappa protein presence.](https://figures.academia-assets.com/72315061/figure_294.jpg)

![[1268] Partially obstructing hematoma in sigmoid colon. prep and technical difficulty, we switched to an adult colonoscope. As a result of continued difficulty, we stiffened the scope, repositioned the patient, applied abdominal pressure, and we were ultimately able to reach the cecum. Upon withdrawal of the colonoscope, a large, nearly obstructing intraluminal hema- toma with no evidence of bleeding was identified in the sigmoid colon. She denied use of NSAIDS, aspi- rin, or other anticoagulation. She was hemodynamically stable throughout the procedure. In the PACU, she never developed abdominal pain or rectal bleeding, and was passing flatus. She was discharged the same day, with instructions to take laxatives and stay on a liquid diet for three days. She remained asymp- tomatic and was having normal bowel movements at day one, three, and seven after colonoscopy. She was referred to hematology to be evaluated for a blood dyscrasia, but none was found. Intramural hematomas of the gastrointestinal tract are unusual. Symptoms are typically non-specific. Patients may present with diminished bowel sounds, obstruction, low grade fever, leukocytosis, and abdominal tenderness, and there can be mild rectal bleeding to hemorrhagic shock. CT scan is diagnostic, although ultrasound and barium enema have been used with success. Little information exists regarding appropriate treatment of intramural hematomas; however, in a stable patient, conservative observation is reasonable.](https://figures.academia-assets.com/72315061/figure_296.jpg)

![[1274] Cecal ulcer biopsy. ulcer, and ESRD s/p two failed renal grafts. Current medications include pantoprazole, sevelamer cayexalate, senna, and metoprolol. On admission, the patient was found to be hypotensive with 1emoglobin (Hb) of 9 g/dl (baseline 10-11 g/dl). His blood pressure responded appropriately to fluic esuscitation. Subsequent EGD revealed a single non-bleeding gastric ulcer (3 mm) in the pre-pylori: egion of the stomach with no stigmata of bleeding. The patient continued to have intermittent episode: »f BRBPR, necessitating multiple blood transfusions, and a colonoscopy was done, revealing evidence o' ‘olitis and localized ulcerations in the proximal ascending colon and cecum status post biopsies. Dur. ng the hospitalization, an angiography was also performed, which revealed active bleeding from ceca ranches of ileocolic artery status post embolization with cessation of bleeding. Biopsy results from the ecal ulcers on colonoscopy revealed single particle of crystalline material in the background of an ulce! onsistent with kayexalate-induced ulcers (Image 1). Many drugs can cause non-specific damage in the arge intestine, including solitary hemorrhages, erosions, ulcers, and inflammation. The pathogenesis o he lesions caused by drugs is highly variable, with toxic injury and vascular insufficiency thought to be he most common. Kayexalate-induced intestinal injury reveals rhomboid or triangular basophilic crys. als adherent to surface epithelium. Kayexalate is a cation exchange resin which acts in the large intestin« »y exchanging sodium ions for potassium ions. The mechanism of mucosal damage is not clear, and i: eported to be more common in patients with renal failure. It is speculated to be caused by its osmotic ction and vasospasm of intestinal vasculature. The patient in this case recovered after discontinuation o cayexalate. This case highlights the importance of medication-induced GI tract injury. Physicians shoulc »e aware of colonic ulceration and ischemia in renal failure patients taking kayexalate.](https://figures.academia-assets.com/72315061/figure_298.jpg)


![[1278A] Cecal ascending colon wall thickening. Purpose: A 66-year-old male with history of CADs/pCABG presents with sudden onset of diffuse abdominal discomfort. Over time, his abdominal pain became focal, sharp and severe in the right lower quadrant. He denied fever, loss of weight or appetite, nausea, vomiting, rectal bleeding, sick contacts and recent travel. He had a normal colonoscopy three years prior to admission. He is a retired meat cut- ter, married, a non-smoker and consumes alcohol socially. On physical exam, he was afebrile, with HR 81, RR16, BP 110/62 with oxygen saturation 97% RA. Respiratory, neurologic exam and cardiovascular exams were unremarkable. Abdomen was soft, normal bowel sounds with right lower quadrant tender- ness, but no rebound or guarding. Normal digital rectal exam. WBC 13.7 with 76% neutrophils. LFT and BMP were unremarkable. CRP elevated to 23.8. CT abd/ pelvis was notable for asymmetric wall thicken- ing involving a portion of the cecum and ascending colon, with likely involvement of the terminal ileum as well. IV levofloxacin and metronidazole were started on admission, and when he did not improve, colonoscopy was performed. At the ileocecal valve, a nodular ulcerated area, suspicious for ischemic colitis, was biopsied. He was discharged on oral levofloxacin and metronidazole. He was re-admitted for targeted antibiotic therapy when biopsies suggested that the ulcer was the result of infection, rather than ischemia or malignancy. PAS and GMS stains were consistent with Actinomycetes, and Penicillin G 5-m units IV Q6H was started. He was discharged with ceftriaxone for ease of home administration for 12 more weeks. A six-week CT showed interval improvement of the cecal and ileal thickening, fully resolved on a 12-week CT scan.](https://figures.academia-assets.com/72315061/figure_301.jpg)



![Abdominal X Ray: Consistent with marked colonic dilation upto 13.5 cm in diameter Computerized Tomography of Abdomen with Oral contrast: Marked colonic gaseous dilation of ascending, transverse and descending colon. Air fluid levels are seen. No bowel wall thickening or pneumatosis [1281B]](https://figures.academia-assets.com/72315061/figure_305.jpg)

![Case: A 24-year-old active duty male deployed in 2011 in support of Operation Enduring Freedom in Afghanistan sustained an improvised explosive device (IED) blast injury complicated by an open left foot fracture and pseudomonas aeruginosa osteomyelitis following internal fixation. He initially had mild ane- mia attributed to polytrauma and osteomyelitis, but, additionally, was noted to have a peripheral eosino- philia of 3706/mcL. A subsequent serologic parasite work-up was negative, as were stool examinations for ova and parasites. He had persistent mild normocytic anemia through 2012 after an elective left below- the-knee amputation for ongoing complications. He re-presented in 2013, complaining of fatigue with vigorous physical therapy. At that time, he had severe iron-deficiency anemia, with hemoglobin 6 g/dL, MCV 66 fL, iron 14 mcg/dL and ferritin 1.8 ng/mL, and ongoing eosinophilia of 2414/mcL. Colonoscopy demonstrated numerous 1.5-cm long worms. Based on exposure in Afghanistan, severity of progressive anemia, gross examination, and four hook-like teeth at the caudal end of the adult worm, Ancylostoma duodenale infection was diagnosed. The patient improved, following treatment with albendazole and iron replacement. While well-described hookworm outbreaks occurred in U.S. forces during the Second World War and, more recently, in Grenada, hookworm infections are rare in contemporary military operations. There are no prior documented cases of Ancylostoma infection in military service members returning from U.S. operational support in the Middle East or central Asia. Comprehensive public health and hygienic practices are necessary to prevent this and other enteric diseases in the deployed setting. [1284] Hookworms visualized during colonoscopy. A worm was removed via biopsy forceps to facilitate identification.](https://figures.academia-assets.com/72315061/figure_307.jpg)

![[1286] ICCC criteria for Cowden syndrome Features observed in the case are mentioned in bold.](https://figures.academia-assets.com/72315061/table_015.jpg)


![[1286] Colonic mucosa with spindle cell proliferation essentially replacing the lamina propria between crypts (200x). demonstrates that this disorder could be more frequent than is currently estimated. A combination of macrocephaly and recurrent gastrointestinal bleeding with skin manifestations should raise suspicions for this disorder. Due to its autosomal inheritance pattern, all family members who have macrocephaly should be evaluated. Screening is important, as there is increased risk for breast (85%), thyroid (35%) and endometrial (28%) cancer. Usual GI manifestations include colorectal hamartomas with esophageal glycogenic acantholysis (seen in this patient), which could be as high as 85%.](https://figures.academia-assets.com/72315061/figure_311.jpg)


![[1296] Table 1. Characteristics of patients and outcome](https://figures.academia-assets.com/72315061/table_016.jpg)





![{1300C] Thickening of submucosal blood vessel walls from amyloid deposition .](https://figures.academia-assets.com/72315061/figure_319.jpg)

![[1300D] Submucosal blood vessels with thickened walls secondary to amyloid deposition. These vessels have been stained with congo red with resulting apple green birefringence under polarized microscopy.](https://figures.academia-assets.com/72315061/figure_321.jpg)
![1303] Multiple small punched-out ulcers seen in the cecum with adherent clot covering one of the ulcers (A). Homeostasis was attempted with placement of two homeostasis ‘lips (B). Case: A 52-year-old female presented for evaluation of abdominal pain. Abdominal CT scan revealed a large polypoid mass in the cecum with heterogeneous enhancement in the center. Multiple enlarged lymph nodes around the mass were noted. CEA level was normal. Colonoscopy showed a lobulated, friable mass arising from cecum. Histopathological evaluation revealed poorly differentiated invasive carcinoma with squamous differentiation. Malignant cells were strongly positive for p63 at the areas of squamous differentiation, scattered malignant cells were positive for CK20 and CDX2. In addition, the malignant cells retained nuclear staining for MLH1, MSH2, MSH6, and PSM2. Surgical exploration confirmed a 12-cm cecal mass infiltrating into the terminal ileum. Open right hemicolectomy with primary ileo-colic anastomosis was performed, and the tumor was staged IIIC with lymph-vascular invasion. Three months after her initial surgery, and before the initiation of the planned adjuvant chemotherapy, the patient underwent repeat surgical exploration for drainage of a fluid collection. At that time, recurrence of the](https://figures.academia-assets.com/72315061/figure_322.jpg)

![[1309B] Spirochetes attached to luminal border of epithelium.](https://figures.academia-assets.com/72315061/figure_324.jpg)
![[1309A] Colonic epithelium showing fuzzy blue line of spirochetes. Reference: [1] Junji Umeno et al. Intestinal spirochetosis due to Brachyspira pilosicoli: endoscopic and radiographic features. J Gastroenterol 2007;42:253-256.](https://figures.academia-assets.com/72315061/figure_325.jpg)


![{1312] Solitary PGN in rectum. Summary: PGN is not associated with increased risk of colon cancer, and doesn't require any further follow-up. GP and DG can be associated with increased risk of colon and other cancers, and patients may benefit from aggressive surveillance.](https://figures.academia-assets.com/72315061/figure_328.jpg)
![[1315] Descending colon polyp and histopathology showing spindle cells and hyperchromatic nuclei. Purpose: Mucosal Schwann cell hamartoma, a rare neural tumor, is rarely found in the colon, yet when seen, it is commonly as a small colorectal polyp, typically on the left side. We report two cases of Schwann ell hamartoma presenting as a polypoid lesion in the proximal colon during routine colonoscopy. Case one: A 78-year-old man with a past medical history of congestive heart failure, hypertension, hyperlipid- >mia, diabetes mellitus type 2, diverticulosis, and peptic ulcer disease presented with hematochezia. His amily history was significant for colorectal cancer in his sister. The patient underwent diagnostic colo- noscopy, which revealed scattered diverticula and a 5-mm sessile polyp at the hepatic flexure. Pathology results from the polypectomy specimen revealed colonic mucosa with stromal proliferation of spindle ells with bland nuclear morphology, consistent with Schwann cell hamartoma. Case two: An 84-year- od man with past medical history of hypertension presented for screening colonoscopy. Colonoscopy revealed hemorrhoids and four polyps. Pathology results revealed that a 10-mm sigmoid polyp was a tubular adenoma, a 5-mm hepatic flexure polyp was a tubular adenoma, and a 5-mm splenic flexure dolyp was inflammatory. The fourth polyp was a 5-mm polyp in the mid ascending colon. The pathol- ogy of this polyp showed colonic mucosa with stromal proliferation of spindle cells with bland nuclear norphology, consistent with Schwann cell hamartoma. Purpose: Malignant melanomas account for 1-3% of all malignant tumors of the gastrointestinal (GI) tract, the majority of which are secondary lesions representing metastatic spread. Primary malignant Vishnu Vandana Palle, MD, Ashutosh Gupta, MD, Victoria Angelova, MD, Asad Rafiq, MD, Bashar Attar, MD, PhD, FACG. John H. Stroger Hospital of Cook County, Chicago, IL.](https://figures.academia-assets.com/72315061/figure_329.jpg)
![[1319] Anorectal melanoma detected on flexible sigmoidoscopy. Purpose: A 77-year-old Caucasian female with past medical history of external hemorrhoids presented with a three-month history of anal pain, mucus discharge, and pruritus. She had also experienced inter- mittent anal spasms made worse by bowel movements. The patient was treated symptomatically with hemorrhoid wipes and sitz baths. Her rectal discharge persisted to the point the patient was requiring pads to protect her undergarments. She eventually detected a noticeable lesion near the anus. Flexible sigmoidoscopy revealed a smooth 3x2-cm dark brown nodule at the anal verge. The patient was referred](https://figures.academia-assets.com/72315061/figure_330.jpg)
![[1322A] Colonoscopy showing large ulcers at the hepatic flexure. Purpose: Case Report: A 71-year-old man presented to the emergency room about 12 hours after insert- ing a perfume bottle into his rectum. Manual self attempts to remove the perfume bottle resulted in the cap getting stuck and moderate rectal bleeding. Patient reported that he had been drinking and snorting cocaine prior. He also reported abdominal pain, flatulence, distention, and the inability to void urine. The patient’s vital signs were: temperature of 97.8°F (36.6°C), pulse of 101, respiratory rate of 16, and blood pressure of 162/87. Abdominal exam revealed a soft, distended abdomen with lower abdominal tender- Introduction: Cytomegalovirus (CMV) gastrointestinal disease is an uncommon but serious complication of acquired immunedeficiency syndrome (AIDS). Recently, the incidence of CMV gastrointestinal disease has decreased substantially since the advent of highly active anti-retroviral therapy (HAART). Case: A 62-year-old male with history of HIV on HAART was sent from a nursing home for evaluation of respiratory distress with oxygen saturation of 89% on room air. On admission, the patient was noted to have supratherapeutic INR of 4.7. The patient was on warfarin for DVT. He was also found to have an acute drop in hematocrit with no obvious source of bleeding. He received packed red blood cells. He also received vitamin K to reverse coagulopathy. While in the hospital, the patient had recurrent episodes of bright red bleeding per rectum. Despite reversing coagulopathy and multiple packed red blood cell transfusions, he became hypotensive. He was transferred to ICU, where he continued to bleed. Colonos- copy was performed. The bowel preparation was suboptimal. The source of bleeding could not be identi- fied. The patient stopped bleeding spontaneously, and was later transferred to the general medical floor. The patient later had another episode of rectal bleeding. A Bleeding scan showed bleeding originating](https://figures.academia-assets.com/72315061/figure_331.jpg)
![Discussion: Rectal foreign bodies are usually a result of deliberate insertion. However, some are a result of assault, iatrogenic, or due to foreign bodies traversing the digestive tract and becoming impacted in the rectum. Presentation usually involves abdominal pain, obstructive symptoms, and rectal bleeding. Per- foration and signs of infection may be evident in complicated cases. Abdominal/pelvic x-rays should be obtained to delineate the foreign body position, shape, size and the presence of pneumoperitoneum. In stable patients without evidence of perforation or peritonitis, digital removal of the foreign body should be attempted first. Low-lying rectal foreign bodies can be removed using one of many clamps and/or instruments. Other methods of removal include endoscopic/fluoroscopic-guided balloon extraction, anal dilation with manual or forceps extraction under anesthesia. Laparotomy is indicated in patients who present with perforation, sepsis, ischemic bowel, or after failed transanal attempts. {1321] Figure. Perfume cap in rectum.](https://figures.academia-assets.com/72315061/figure_332.jpg)
![[1322B] Histopathology: colonic mucosa showing giant cells with pleomorphic basophilic inclusion bodies (Owl’s eyes)and inflammatory cells.](https://figures.academia-assets.com/72315061/figure_333.jpg)
![[1326A] Figure 1. Image depicts a friable, obstructive mass in the sigmoid colon.](https://figures.academia-assets.com/72315061/figure_334.jpg)
![[1326B] Figure 2. Tumor consists of high grade pleomorphic cells arranged in pseudo-papillary clusters within stromal spaces resembling vascular spaces. The tumor cells lack fibrovascular cores and displays reverse cell polarity. Mitotic figures are few and the tumor lacks the “dirty necrosis” seen in conventional adenocarcinoma of the colon.](https://figures.academia-assets.com/72315061/figure_335.jpg)

![[1340] Colonic wall thickening and mucosal ulceration. Purpose: Stercoral colitis is an uncommon inflammatory condition of the colonic wall, related to fecal impaction and resulting in ischemic pressure necrosis and ulceration. It differs from other forms of colitis by the clinical absence of diarrhea. This case highlights the potentially fatal nature of this condition if not diagnosed and treated promptly. A 27-year-old woman was evaluated for a six-week history of constipa- tion, abdominal pain, and distension. She denied vomiting or passage of flatus, and had unsuccessfully tried multiple bowel agents. Her medical history included obstipation and bipolar disorder treated with gabapentin and trazodone. She appeared to be in painful distress with an obese, soft, and diffusely tender abdomen without guarding or rebound. Rectal exam, though limited by patients discomfort, reported a large, firm fecal mass within the anal verge. Basic laboratory testing was unremarkable, and a plain abdominal film showed a large amount of colonic stool. An enhanced computed tomography (CT) of the abdomen and pelvis confirmed a significant amount of colonic stool with marked rectal distension, focal colonic wall thickening, mucosal ulceration, and stranding of pericolonic fat. She underwent aggressive bowel cleansing and colonic disimpaction under sedation. Flexible endoscopy demonstrated a solitary, non-bleeding ulcer on the anterior rectal wall just proximal to the dentate line. Consequently, she was](https://figures.academia-assets.com/72315061/figure_338.jpg)
![[1341] Mass in the cecum. Discussion: Very few cases of ischemic colitis resembling colon cancer have been reported. Almost all cases reported were initially misdiagnosed as colon cancer, based on endoscopic findings, but endoscopic biopsy confirmed ischemic colitis. Our case had such severe cellular atypia that this differentiation could not be made. In such circumstances, a high index of suspicion with additional review of biopsy speci- mens might help in confirming the diagnosis and avoiding unnecessary surgery.](https://figures.academia-assets.com/72315061/figure_339.jpg)



![[1356] Surgical resection: colonic lipoma at site of intussusception.](https://figures.academia-assets.com/72315061/figure_343.jpg)



![[1367] Langerhans cell histiocytosis in a colonic polyp. Purpose: Langerhans cell histiocytosis (LCH) is a rare disorder of unknown pathogenesis. It is charac- terized by abnormal proliferation and dissemination of Langerhans cells, which are derived from the bone marrow. The disease most commonly affects the bones and the skin. Involvement of the GI tract is extremely rare. We report a case of isolated LCH in a colonic polyp. A 49-year-old woman presented with complaints of constipation, abdominal bloating, and mild change in bowel habits. She denied abdominal pain, early satiety, or weight loss. Family history was positive for colon cancer in her mother and mater- nal aunt. Physical exam was non-revealing. She underwent a diagnostic colonoscopy, which showed three diminutive polyps at the splenic flexure. These were removed by cold biopsy polypectomy. The rest of the colon exam was unremarkable. On histology, one of the polyps showed an ovoid collection of atypical cells within the submucosa. The cells were intermediate in size with eosinophilic cytoplasm and ovoid nuclei. The nuclei were convoluted. No cytoplasmic inclusions were identified. The atypical cells extended into the lamina propria. Immunohistochemical staining showed the cells to be strongly positive for CD1a and $100, which confirmed the diagnosis of LCH. The other polyps were hyperplastic. Sub- sequent extensive clinical work-up showed no evidence of disseminated LCH. Only mild eosinophilia (10.3% eosinophils) was evident. Liver function tests and urinalysis were normal. Chest x-ray showed no acute disease. CT chest showed no pulmonary lesions suggestive of Langerhans cell histiocytosis. There was no mediastinal lymphadenopathy. Review of published literature shows only a handful of cases of colonic involvement with LCH in adults. Most patients are either asymptomatic or have nonspecific GI symptoms. Polyps have usually been found incidentally on screening colonoscopy. The polyps are reported as small (less than 1 cm) and solitary, as in our patient. Only two patients have been reported to have progressed to multisystem disease with skin involvement.](https://figures.academia-assets.com/72315061/figure_347.jpg)
![[1370] CT scan of the abdomen without contrast showed mass in the cecal regior eroding through the abdominal wall with gas in the abdominal wall.](https://figures.academia-assets.com/72315061/figure_348.jpg)

![[1378A] CMV stain showing CMV in brown. Purpose: A 66-year-old man with HTN was initially admitted for pancolitis and diarrhea, found to have a DVT, was initially discharged on empiric antibiotic therapy, only to return with continued bouts of diarrhea, despite radiographic resolution of pancolitis on a return hospital admission. After ruling common microbial etiologies for diarrhea by medication reconciliation and HIV testing, a colonoscopy revealed ulcerations. Pathology and histological staining of the biopsy confirmed the diagnosis of CMV colitis. Subsequent hospitalization, the patient's condition improved with conservative management and supportive care. CMV is a well-known opportunistic viral infection in immunocompromised patients. However, immunocompetent individuals may occasionally be infected with CMV colitis as well. GI tract](https://figures.academia-assets.com/72315061/figure_350.jpg)
![{1378B] CMV infected cells with “Owl Eye” inclusion bodies. (GIT) and CNS are the most frequent sites of CMV infection in immunocompetent adults (1,2,3). The most common site of GIT involvement is the colon. Another well known complication of CMV infectior in the immunocompetent population is the development of DVT (4). CMV can be a secondary pathoger that is superimposed on chronic, pre-existing disease in the gastrointestinal tract. Because of its lov incidence, CMV is not among the primary differentials in patients presenting diarrhea in immunocom. petent patients (5,6,7). However, clinicians should suspect CMV colitis in immunocompetent patient: who have negative stool studies and are refractory to empirical antibiotics therapy. Due to the irritating effects of CMV to the mucosa, as well as the vasculature, it is important clinicians maintain a high inde of suspicion for such a case (5).](https://figures.academia-assets.com/72315061/figure_351.jpg)


![[1390] Endoscopic view of the bleeding lesion at 35 cm. Purpose: A 79-year old female presented with a one-day history of rectal bleeding. Of note, she had a his ory of atrial fibrillation on dabigatran for anticoagulation. Her admission hemoglobin was normal, anc she was empirically started on a proton pump inhibitor drip and IV fluids. It was recommended that sh ‘eceive FFP for reversal of the anti-thrombin effects of dabigatran; however, she was a Jehovah's Witnes ind refused. CT scan revealed a focal fluid collection near the rectum, thickening of the rectal mucosa ind diverticulosis. Colon prep was initiated in anticipation of both upper and lower endoscopy. Uppe endoscopy revealed a 10-cm sliding hiatal hernia and erosive gastritis, with no stigmata of recent bleed ng. Colonoscopy revealed an ulcerated, round shaped, actively bleeding lesion at about 35 cm from th inal verge. Hemoclip placement was attempted, but the mucosa was too friable. Epinephrine was injectec nto the surrounding mucosa with improved hemostasis. General surgery performed a Hartmann’s pro -edure, and during the operation, the surgeon noted that there were two lesions (one at 35 cm anc nother at 8 cm from the anal verge) seen originating from the external wall of the colon of white anc ‘ed color, both eroding through the wall of the colon and both actively bleeding at that time. The initia surgical opinion was that the lesions represented endometriosis. Surgical pathology supported metastati s0orly-differentiated carcinoma involving only the serosa, highly suggestive for a gynecologic primar both lesions were negative for TTF-1, CK20, and CDX2 immunostains, and strongly positive for p53 WT-1, estrogen receptor, and CK7 immunostains). Both lesions also exhibited strongly positive nuclea staining for PAX-8, highly suggestive of metastatic ovarian serous carcinoma. This case represents a ver inusual cause of lower gastrointestinal bleeding. While metastatic ovarian carcinoma involving the colot 1as been reported, it is rare for it to present initially as profuse rectal bleeding without any alarm symp oms in an otherwise healthy patient. The fact that there was two separate metastatic lesions, both of iden ical immunochemical makeup and located such a distance apart, also makes this case very interesting.](https://figures.academia-assets.com/72315061/figure_354.jpg)

![[1402] Computed tomography of the chest with intravenous contrast showed the presence of bilateral lower lobe infiltrates and trace pleural effusion. Discussion: The exact pathophysiology of mesalamine-induced lung injury is not known. It is important to distinguish pulmonary manifestations in patients with IBD secondary to drug-related Case Presentation: A 65-year-old man presented with intermittent low-grade fever, non-productive cough and exertional shortness of breath for a period of week. The patient had been diagnosed with ulcerative colitis (UC) 2 weeks prior during an outpatient evaluation for chronic bloody diarrhea. He was started on therapy with mesalamine 1.2 gm four times daily. On physical examination, the patient was febrile, tachycardic and tachypneic. Arterial blood gas values revealed a ph of 7.50, pCO2 of 20 mmHg, PO, of 70.7 mmHg and bicarbonate level of 19 mmol/L on 2 L oxygen. Computed tomography of the chest showed bilateral lower lobe infiltrates with trace pleural effusions (Figure1). Mesalamine was discontinued and intravenous antibiotics were initiated. However, the patient devel- oped worsening respiratory distress and was intubated later the same day. A transbronchial biopsy was performed, which revealed interstitial lymphocytic infiltrates, few histiocytes and mild fibrosis. A diagnosis of drug-induced interstitial pneumonitis was made and intravenous corticosteroids were started. The patient showed gradual clinical improvement, was extubated four days later and dis- charged on oral prednisone.](https://figures.academia-assets.com/72315061/figure_356.jpg)
![{1403A] Figure 1. Cecum at day O. Conclusion: To our knowledge, this is the first report of complete mucosal healing following a single FMT infusion in an IBD patient. These results suggest that FMT may be a promising therapy in < subgroup of IBD patients. Further research is needed to further characterize the IBD population most likely to benefit from FMT.](https://figures.academia-assets.com/72315061/figure_357.jpg)

![[1403B] Figure 2. Cecum at day 28 following FMT.](https://figures.academia-assets.com/72315061/figure_358.jpg)
![[1405A] Case 1: Severe inflammation at 120cm (water-filled lumen).](https://figures.academia-assets.com/72315061/figure_359.jpg)
![[1405B] Case 2: Inflammation, ulceration of transverse colon (water-filled lumen). [1406A] Figure 1.](https://figures.academia-assets.com/72315061/figure_360.jpg)
![[1405C] Case 3: Colitis, pesudopolyps near ileocecal valve. {1406B] Figure 1.](https://figures.academia-assets.com/72315061/figure_361.jpg)





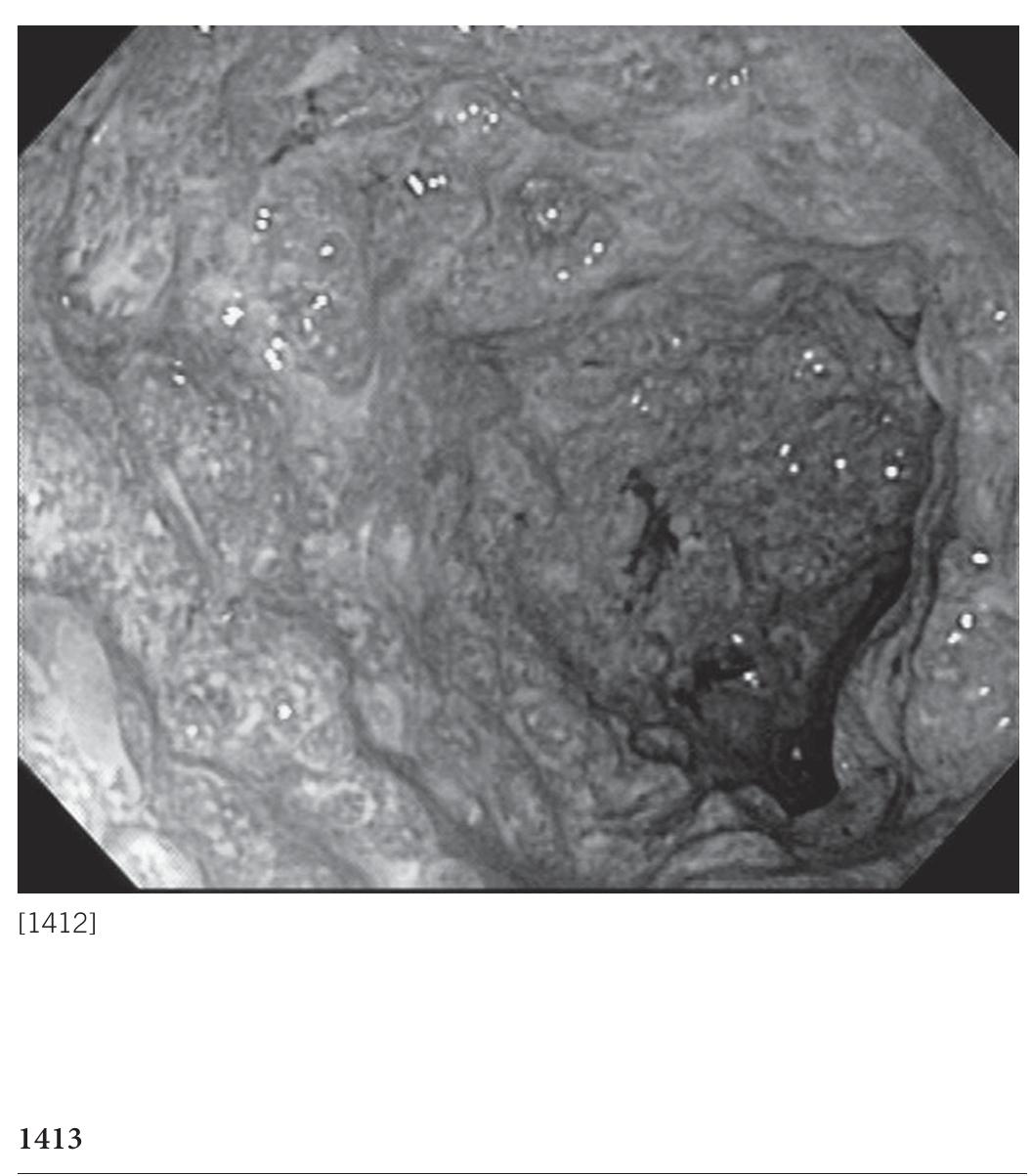

![[1422] Table 1. Reported cases of collagenous colitis evolving into ulcerative colitis](https://figures.academia-assets.com/72315061/table_018.jpg)
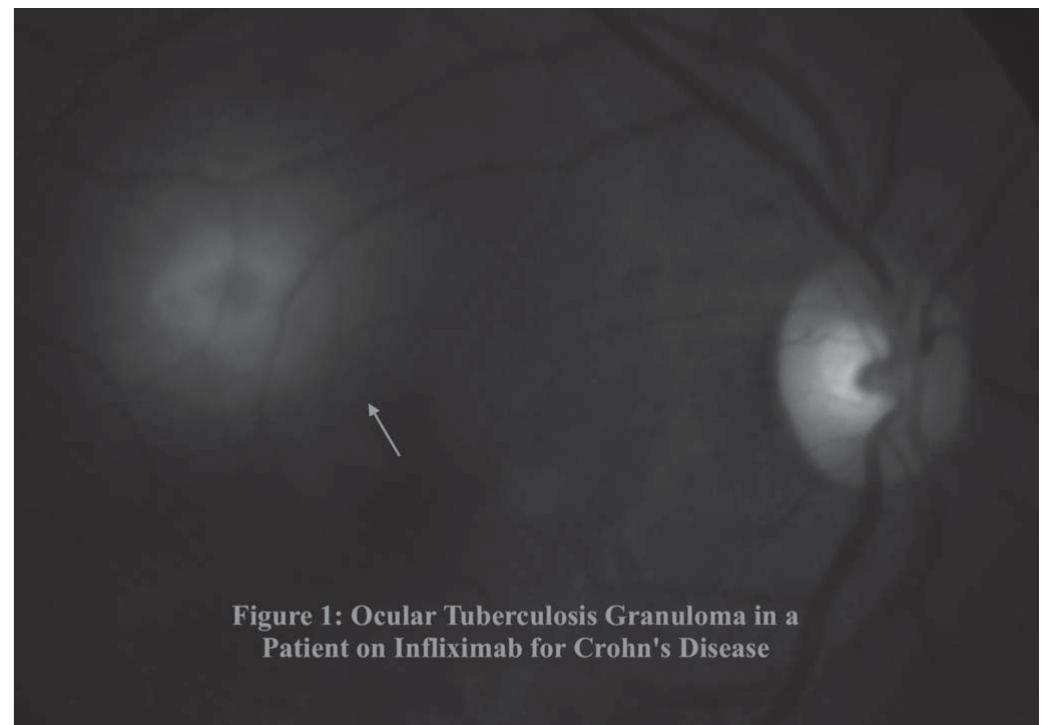

![[1446A] Figure 1. Leg wound at time of presentation. Purpose: A 70-year-old male presents with a week-long course of severe non-bloody watery diarrhea and is discovered on admission to also have a large poorly-healing lower extremity ulceration (Figure 1) for which he has had chronic wound debridement for the past 6 months. He denies any diarrhea prior to a week ago, or constitutional symptoms. His last colonoscopy was within the past year which was normal. His leg wound initially presented 6 months ago as a red bump on his right lower leg which rapidly enlarged and ulcerated over the course of 1 month. Initially this wound was presumed to be infectious but failed to respond to antibiotics. Vascular studies were normal. Over the next five months Purpose: A 48-year-old man with no significant past history was evaluated by gastroenterology 3 years ago for a history of acute diarrhea, chronic perirectal fistula and abscess. Colonoscopy showed exten- sive pancolitis with innumerable apthous ulcers and pseudopolyps. No fistulous tracts were noted in](https://figures.academia-assets.com/72315061/figure_371.jpg)
![[1446B] Figure 2. Leg wound at 4 months of treatment.](https://figures.academia-assets.com/72315061/figure_372.jpg)

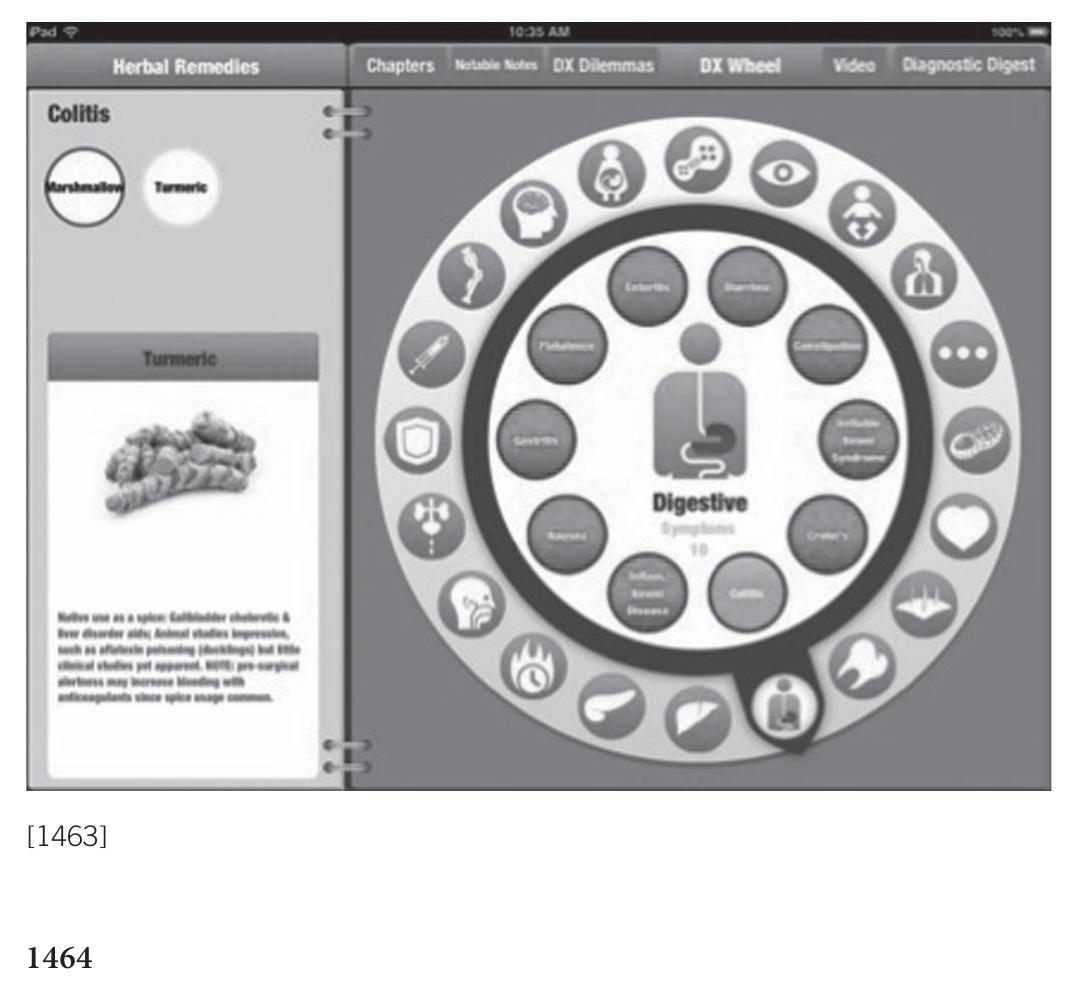

![[1473A] A lesion seen in the terminal ileum. Discussion: We report a case of BRBNS presenting as symptomatic anemia. Treatment options are lim- ited for this rare GI hemangioma syndrome, and usually consist of supportive and conservative manage- ment. Iron supplementation and transfusions for symptomatic anemia are the mainstay of therapy, but if recurrent bleeding occurs, endoscopic and surgical treatment may be warranted, as medical options have shown little, if any, proven benefit.](https://figures.academia-assets.com/72315061/figure_376.jpg)
![[1473B] A lesion with no bleeding was noted in the 1st portion of the duodenum.](https://figures.academia-assets.com/72315061/figure_377.jpg)
![[1475] Indications for percutaneous feeding tube insertion with related pre-pregnancy variables and post-pregnancy outcomes](https://figures.academia-assets.com/72315061/table_019.jpg)
![[1476A] Cross section CT scan of the abdomen before and after colonoscopy; Image on the right shows hemoperitoneum and a ruptured spleen. Purpose: Colonoscopy is a safe procedure that is performed routinely worldwide. There is, however, < small but significant risk of splenic injury, as this case report highlights. A 73-year-old female with a his- tory of small bowel obstruction status post small bowel resection underwent colonoscopy for work-uf of anemia. Colonoscopy revealed severe diverticulosis in the sigmoid, descending and transverse colon Small sessile polyps were found in the sigmoid, ascending, and descending colon, and were removed vie cold and hot snare technique. Post-procedure, the patient developed abdominal pain, became hypoten- sive and had a drop in her hemoglobin. CT revealed a 13.9 x 9.5 x 12.9 cm clot in left upper quadrant](https://figures.academia-assets.com/72315061/figure_378.jpg)
![[1476] Cases of splenic rupture following a medical procedure NO ee tT ONT ne WS GR TT TO ET TAS NT RNS A SH oe I Tene ETC IE NIVEA TN NC SEER TENN we ON oo OE Ane van TE RTT REN Sara Ancello, DO,' Ricardo Prieto Roig, MD,’ Jon Finan, MD, PhD,? Patrick Brady, MD, FACG’. 1. University of Medicine and Dentistry of New Jersey School of Osteopathic Medicine, Stratford, NJ; 2. University of South Florida, Tampa, FL.](https://figures.academia-assets.com/72315061/table_020.jpg)
![[1476B] CT Scan showing the post-splenectomy splenic bed.](https://figures.academia-assets.com/72315061/figure_379.jpg)
![[1477B] Polyp in the duodenum. [1477A] IFP prolapsing through the pylorus.](https://figures.academia-assets.com/72315061/figure_380.jpg)

![[1477C] H&E stain shows spindle shaped cells and a background of inflammatory cells with increased eosinophils.](https://figures.academia-assets.com/72315061/figure_382.jpg)

![[1482A] Figure 1. Endoscopic images: one clip placed proximal to duodenal lesion, and 2. clips placed distally to jejunal lesions.](https://figures.academia-assets.com/72315061/figure_384.jpg)
![{1482B] Figure 2. CT Simulation: The red volume is the gross tumor volume while the magenta represents the Planning Target Volume which accounts for error due to motion and technique. Note the location of the clips acting as fiducials for future radiation.](https://figures.academia-assets.com/72315061/figure_385.jpg)
![Abbreviations: EGD, esophagogastroduodenoscopy; IC, ileocecal; IV, intravenous; TI, terminal ileum. [1483] Table 1. Comparison of the two methods of colonoscopy used in the same patient](https://figures.academia-assets.com/72315061/table_021.jpg)
![[1483] Water-filled distal small bowel at ~100 cm from IC valve.](https://figures.academia-assets.com/72315061/figure_386.jpg)
![[1484] Fig A. Close proximity of mucosa to polyp at the beginning of water infusion. Fig B. Snare in position to capture polyp in the center of the water-filled lumen. Fig C. Polyp snared off stalk, cut end is seen. Fig D. Snared polyp captured in basket.](https://figures.academia-assets.com/72315061/figure_387.jpg)
![[1485] Partially-covered metal stent in the distal esophagus (A). Six weeks after placement (B). Fully-covered metal stent placed within the partially-covered metal stent (C). Endoscopic appearance after stents removed. Residual surgical suture, arrow (D).](https://figures.academia-assets.com/72315061/figure_388.jpg)
![[1486] Diffuse portal venous gas is seen throughout the right hepatic lobe extending to the periphery of the liver. Purpose: Hepatic portal venous gas (HPVG), a rare condition in which gas accumulates in the portal venous circulation, is often associated with significant underlying pathology such as intestinal ischemia, inflammatory bowel disease, sepsis and trauma. HPVG after endoscopic procedures is an unusual com- plication. A healthy 34-year-old male with a past medical history significant for eosinophilic esophagitis presented to his physician with dysphagia to both liquids and solids. Subsequently, he underwent upper endoscopy for further evaluation. Upper endoscopy revealed esophageal mucosal changes suggestive of eosinophilic esophagitis including loss of vascular pattern and whitish exudates along the middle third of the esophagus. A benign-appearing stricture was also noted at the gastroesophageal junction. This stricture was dilated with a balloon size of 18 mm. Biopsies were taken to confirm the diagnosis of eosin- ophillic esophagitis. The procedure was then terminated with no noted complications. However, post procedurally the patient experienced significant nausea and epigastric pain. Physical exam demonstrated diffuse epigastric tenderness to palpation with no guarding or rigidity. Laboratory work-up revealed a normal complete blood count as well as normal liver and pancreatic enzymes. Computerized tomogra- phy demonstrated diffuse portal venous gas throughout the right hepatic lobe extending to the periphery of the liver (Figure 1). The patient was admitted for observation and treated conservatively with IV fluids and pain control. He was discharged the following day with resolution of his symptoms. Follow-up CT scan revealed no residual portal vein air and he continues to do well at 6 months. This case highlights an unusual complication of HPVG after upper endoscopy and dilation and the role of conservative man- agement. As endoscopy continues to serve as a therapeutic role in management of many GI disorders, potential for an increase in complications is likely. Recognition of HPVG as a transient complication is critical to guiding appropriate therapeutic management.](https://figures.academia-assets.com/72315061/figure_389.jpg)



![[1489A] Gastric dehiscence/perforation. Conclusion: Endoscopic stenting of a gastric perforation/dehiscence as large as 5.0 cm with complet: healing and closure is achievable with esophageal wall stents that are fully covered and secured with resolution clips.](https://figures.academia-assets.com/72315061/figure_393.jpg)
![{1489B] Two overlapping stents: GEJ to duodenal bulb.](https://figures.academia-assets.com/72315061/figure_394.jpg)



![Histological and endoscopic gastric and duodenal images showing pseudomelanosis. [1496] Table 2. Histopathological features](https://figures.academia-assets.com/72315061/table_022.jpg)
![[1496] Table 1. Demographics, clinical features, and lab values of patients with pseudomelanosis](https://figures.academia-assets.com/72315061/table_023.jpg)
![[1496] Histological and endoscopic gastric and duodenal images showing pseudomelanosis.](https://figures.academia-assets.com/72315061/figure_398.jpg)
![[1497A] Colonoscopy with normal mucosa.](https://figures.academia-assets.com/72315061/figure_399.jpg)
![[1497B] Endoscopy with normal mucosa.](https://figures.academia-assets.com/72315061/figure_400.jpg)
![[1502] Left image: Gentle rotation of stent retriever. Right image: Central defect after distruption with stent retriever.](https://figures.academia-assets.com/72315061/figure_401.jpg)

![[1507] Multiple, flat, punctate melanoma lesions in the gastric body. the spectrum of recurrent disease. Metastatic gastric melanoma typically presents as a single or multiple polypoid lesions. We report a case of metastastic melanoma with the unusual endoscopic appearance of diffuse, flat, punctuate lesions throughout the stomach. A 79-year-old man with a distant history of choroidal melanoma treated with brachytherapy, was admitted to the hospital by his cardiologist with complaints of worsening fatigue and nausea. Prior to his presentation to the hospital, he had also noted mild right-sided abdominal pain, and a CT scan (done without IV contrast because of renal insufficiency) was unrevealing. In addition to a cardiac work-up and telemetry monitoring while in the hospital, an ultrasound of the abdomen was obtained. Ultra- sound revealed a mass measuring 9.4 x 7.8 x 10.3 cm in the right lobe of the liver with other smaller, hypoechoic masses throughout the liver that were suspicious for metastases. The patient had a normal colonoscopy within the last 3 years. Subsequent esophagogastroduodenoscopy revealed multiple flat, black, punctate mucosal lesions throughout the stomach with intervening areas of normal mucosa in the fundus, body and antrum. Gastric biopsies of these black lesions confirmed metastatic melanoma. Ocular and head and neck melanomas have a predilection to metastasize to the liver. However, malignant melanoma metastasizing to gastrointestinal tract is rare. Gastric metastases have a poor prognosis with 50% of patients surviving for less than 12 months. Endo- scopically, metastatic melanoma can appear as a single lesion similar to gastric adenocarcinoma, as multiple ulcerated polypoid lesions or less commonly as a small mucosal lesion. Our case rep- resents a rare endoscopic presentation of multiple, small, flat, punctate lesions throughout the stomach. The diagnosis of melanoma should be considered when such lesions are encountered on upper endoscopy.](https://figures.academia-assets.com/72315061/figure_403.jpg)
![[1508B] PD stent and mucosal changes after thermal coagulation.](https://figures.academia-assets.com/72315061/figure_404.jpg)
![[1508A] Figure A: EGD showing bleeding from the papilla.](https://figures.academia-assets.com/72315061/figure_405.jpg)
![[1509] Histological and endoscopic appearance of duodenum in leishmania. Jawher and Valenzuela et al, they describe a whitish discoloration of mucosa with nodularity simila1 in appearance to our case. Marked infiltration of mucosa with protozoan laden macrophages result: in poor visualization of submucosal blood vessels leading to loss of normal pink color of the mucosa The severity of loss of normal endoscopic pattern may also parallel the disease severity in the mucosa The major differential diagnosis of nodular white duodenal mucosa is Whipple’s disease. The histol- ogy in both diseases is infiltration of mucosa by organism-containing macrophages, hence simila1 appearance of mucosa is seen on endoscopy. The appearance of a whitesh, nodular mucosa on endos- copy should raise suspicion of duodenal leishmaniasis versus Whipple's disease in the appropriate clinical settings.](https://figures.academia-assets.com/72315061/figure_406.jpg)
![[1510] Anastomotic bands. Conclusion: We reported a unique case of anastomotic site small bowel obstruction caused by translumi nal mucosal bands, treated successfully by novel through scope thermal ablation.](https://figures.academia-assets.com/72315061/figure_407.jpg)


![[1520A] Figure 1: a. Upper endoscopy showing giant folds in body of stomach, b. Metastatic adenocarcinoma in the stomach (200x), c. Immunohistochemical staining for prostate specific antigen (PSA) highlights the malignant cells.](https://figures.academia-assets.com/72315061/figure_410.jpg)
![1520B] Figure 2: a. Colonoscopy showing circumferential nodular mucosa and poor distensibility of the rectum, b. High-grade prostatic carcinoma in rectal biopsy (200x), c. - SA stain also show few positive malignant cells.](https://figures.academia-assets.com/72315061/figure_411.jpg)
![[1523A] The transparent cap slipped off the distal end of the endoscope and the hot biopsy forceps was introduced to catch it. Conclusion: Transparent cap slip during POEM could be treated by use of hot biopsy forceps. Results: Finally, the entry incision was well closed by endoscopic clips and the post-POEM X-ray did not expose complications like pneumothorax or pneumomediastinum. One week after POEM, dysphasia was relieved and the patient was discharged after a routine endoscopy assuring the complete closeness of the entry of the submucosal tunnel. cee lms mn ts rs eee of x we aig ycapstg: ‘*:](https://figures.academia-assets.com/72315061/figure_412.jpg)

![[1523B] The transparent cap was retracted out of the submucosal tunnel into the esophageal lumen.](https://figures.academia-assets.com/72315061/figure_414.jpg)
![EUS Use in Proinsulinomas: Diagnosis and Localization with Fiducial Markers Jeffrey Juneau, MD, Ioana Smith, MD, Brandi Blackburn, MD, Shabnam Sarker, MD, Ali Khan, MD, Jessica Tracht, MD, Jessica Trevino, MD. University of Alabama at Birmingham, Birmingham, AL. {1527C] Intraop US revealing the proinsulinoma and fiducial markers.](https://figures.academia-assets.com/72315061/figure_415.jpg)

![[1527A] A) Histopathologic examination reveals a solitary, encapsulated, well-differentiated neruoendocrineneoplasm. NI pancreatic parenchyma is present, adjacent to the tumor. B) Tumor consists of trabeculae architecture with uniform neuroendocrine cells showing low-grade nuclear features and cytoplasmic neurosecretory granules. Amyloid deposits are seen t/o the tumor nests. C) Immunohistochemistry for Ki-67 is reactive in <2% of cells, consistent with a grade 1 neuroendocrine tumor.](https://figures.academia-assets.com/72315061/figure_417.jpg)
![[1527B] A) Cytopathologic examination with diff-quick stain reveals a loosely cohesive, monotonous population of cells with round nuclei and scant poorly defined cytoplasm con- taining neurosecretory granules. Immunohistochemistry performed on cell block preparation is reactive for both chromogranin (B) and synaptophysin (C).](https://figures.academia-assets.com/72315061/figure_418.jpg)
![[1528] Figure 1: Retroflexed view showing Mallory-Weiss tears. Purpose: Transesophageal echocardiography (TEE) is a safe, minimally invasive procedure widely used to evaluate cardiac conditions. Complications are rare. An 81-year-old hospitalized female was referred for TEE to exclude infective endocarditis after isolation of methicillin-resis- tant Staphylococcus aureus despite intravenous vancomycin administered for a septic joint. The patient was stable post-procedure, without nausea and vomiting. Three days after, she developed profound hematemesis without antecedent vomiting. Gastric aspiration via NG tube revealed 150 cc of bright red blood. The patient became hypotensive, with a blood pressure of 66/48 mmHg with a drop in hematocrit to 25.4%. Emergency EGD revealed active bleeding and a 10-cm-long clot extending proximal from the GE junction to the distal esophagus. Interventional angiogra- phy with coil embolization of left and right gastric arteries failed to arrest the bleed. Emergency EGD performed for continued bleeding revealed two vertical linear Mallory-Weiss tears at the GE junction with no active bleeding but with stigmata of recent hemorrhage consisting of a blood clot in the lower third of the esophagus. The lesion was treated with heater probe therapy of 6 pulses of 20 joules each with successful cessation of bleeding. The patient died from bowel necrosis secondary to hypovolemic shock from the bleeding. Mallory-Weiss tears after TEE are rare and occur mostly in patients who are anticoagulated postoperatively after TEE performed during cardiac surgery. The mechanism involves trauma by the echoprobe and/or ultrasonic thermal injury. Only a few complications have been reported from diagnostic TEE in nonsurgical patients. Min et al. (J Am Soc Echocardiogr 2005) reported a .03% rate of esophagogastric trauma among 10,000 procedures, further validating the safety of TEE. The present case describes an otherwise healthy elderly female, who experienced fatal upper gastrointestinal bleeding from Mallory-Weiss tear from TEE despite no known gastrointestinal abnormalities and despite not being anticoagulated. This case extends the clinical spectrum of Mallory-Weiss tears from TEE.](https://figures.academia-assets.com/72315061/figure_419.jpg)
![MTaAnQlOMla FF YOSCIMCUI. £1 NATO DUOIOSY OF ATASULOMNOSUTIaL DICCQLIS Christopher Brown, MD, Harshit Khara, MD, Mark Metwally, MD, Maged Bakr, MD, Dennis Meighan, DO, William Hale, MD, FACG, Rakhee Mangla, MD. Department of Gastroenterology ¢& Hepatology, Yale University School of Medicine - Norwalk Hospital, Norwalk, CT. References: [1] Tagg, W et al. Hemoperitoneum after colonoscopy. Endoscopy 2008;40 (suppl 2):E136-7. doi: 10.1055/s-2007-995715. [2] Fusaroli, P et al. Ovarian tumor rupture causing massive hemoperito- neum: an unusual complication of colonoscopy. Gastrointest Endosc 2008;67(7):1177; discussion 1178. doi: 10.1016/j.gie.2007.12.045.](https://figures.academia-assets.com/72315061/figure_420.jpg)
![[1531] Barium swallow image showing esophageal FCSEMS vovering fistula tract and and IR pigtail catheter placed into abscess. Conclusion: Esophageal fistula formation is a known complication of chemo and radiation ther- apy. There are several studies that document effectiveness of using FCSEMS in treating these fistulas. We present a rare case with impressive clinical and endoscopic findings in which a com- bined GI-IR approach helped treat an esophageal fistula causing significant pulmonary symp- toms, and then also eventually improved the patient’s quality of life by allowing him to once again tolerate PO.](https://figures.academia-assets.com/72315061/figure_421.jpg)
![[1535] Sequence of endoscopic therapy. >urpose: A 19-year-old male presented with nausea, vomiting, and epigastric pain. He had a recent listory of NSAID-related perforated prepyloric ulcer with omental patch repair. EGD revealed < in-hole sized pylorus, likely related to scarring from peptic ulcer disease and recent surgery ‘he narrow pylorus could not be traversed. Balloon dilation was performed to 10 mm. Biopsies vere negative for H. pylori. High dose PPI therapy was continued. Two more endoscopies over 5 veeks showed persistent pyloric stenosis and dilation was performed to 15 mm. A fourth endos- opy was performed 3 months from initial presentation, again demonstrating a stenosed pylorus vith inability to pass the endoscope into the duodenum. Balloon dilation was again performec o 15 mm. This time, 4 mL of 10 mg/mL solution of triamcinolone acetonide was injected in our quadrant fashion into the stricture. Follow-up EGD 3 months later showed marked improve- nent in the appearance of the pylorus, which was now patent. The endoscope easily traversed he pylorus. The patient is asymptomatic on a general diet at 10 month follow-up. Endoscopic alloon dilation is the first-line therapy for patients with benign acquired pyloric stenosis atients who require more than two dilations are at high risk of endoscopic failure and need fo1 urgical intervention. Endoscopic balloon dilation combined with intralesional steroid injec- ion may be an effective alternative to surgery in such patients. Intralesional steroid inhibit: tricture formation by interfering with collagen synthesis, fibrosis and chronic scarring rocesses. Triamcinolone inhibits the transcription of matrix protein genes, including fibronectin nd pro-collagen. It also reduces the synthesis of a2-macroglobulin, an inhibitor of collagenase ctivity. It prevents the cross-linking of collagen which results in scar contracture, so that if the car is stretched and corticosteroid is injected into it, contracture will presumably not occur Yorticosteroids also decrease the fibrotic healing that appears to occur after dilation. To ow nowledge, this is only the sixth reported case of treatment of benign refractory pyloric stenosi: vith intralesional steroid injection.](https://figures.academia-assets.com/72315061/figure_422.jpg)


![[1543] Diverticula in transverse colon. regimen. It is the intent of this report to describe a possible association between DiGeorge syndrome and the co-occurrence of diverticula in such patients.](https://figures.academia-assets.com/72315061/figure_425.jpg)
![[1545] Abdominal CT scan: A hypodense, homogeneous mass with fat stranding in the left upper quadrant consistent with idiopathic segmental omental infarction. Conclusion: Healthcare providers should be aware of the possibility of a left sided OI when presented with a child with complaints of acute left sided abdominal pain. The clinical symptoms when com- bined with CT findings allow for prompt diagnosis and conservative treatment; potentially avoiding unnecessary tests and surgical procedures.](https://figures.academia-assets.com/72315061/figure_426.jpg)
![[1548] EUS image of the cyst. Conclusion: It is extremely difficult to make a definitive diagnosis preoperatively just based on imaging findings, since at first it was thought to be a gastric duplication cyst. This rare clinical entity of a broncho- genic cyst of the stomach was identified by pathological examination only after surgical resection.](https://figures.academia-assets.com/72315061/figure_427.jpg)


Related papers
International Journal of Case Reports and Images, 2017
International Journal of Case Reports and Images (IJCRI) is an international, peer reviewed, monthly, open access, online journal, publishing high-quality, articles in all areas of basic medical sciences and clinical specialties. Aim of IJCRI is to encourage the publication of new information by providing a platform for reporting of unique, unusual and rare cases which enhance understanding of disease process, its diagnosis, management and clinico-pathologic correlations. IJCRI publishes Review Articles, Case Series, Case Reports, Case in Images, Clinical Images and Letters to Editor.
Diseases of the Colon & Rectum, 1986
European review for medical and pharmacological sciences, 2009
Amyloidosis is a rare disease caused by extracellular deposits of insoluble fibrillar proteins in various organs and tissues. There are different forms of amyloidosis distinguished by the type of protein fibrils, by the sites of deposition and by associated conditions. Gastrointestinal involvement is common both in primary and secondary amyloidosis, while isolated gastrointestinal amyloidosis is rare. We describe a case of AL amyloidosis with a gastrointestinal involvement and restrictive cardiomiopathy. A 64 year old woman came to our attention with a history of chronic diarrhoea and weight loss, associated with dysphagia, dry mouth, xerophtalmia, chronic gastritis and depression. Clinical diagnosis has been difficult because of aspecificity of symptoms that mimed other more common diseases, like gastro-paresis, epigastric discomfort, gastric or duodenal ulcers, perforation, malabsorption, intestinal pseudo-obstruction. There is an important risk of misunderstanding and diagnostic ...
Inflammatory Bowel Diseases, 2001
Background: Amyloidosis (A) is a well-known but rare complication to inflammatory bowel disease (IBD). We describe 18 patients with IBD and A, with special emphasis on clinicopathologic features and site relationships, comparing our results with previously reported cases in the world literature. Methods: Patient records were collected from the files of the medical department at Rikshospitalet. Clinical data were compiled from records. Results: Fifteen of the 18 patients had Crohn's disease (CD), 1 had ulcerative colitis (UC), one had UC preceding CD, and 1 had indeterminate colitis. There was a male preponderance of 13:5 ס 2.6. Five of the patients had A at the time of diagnosis of IBD. Median time from diagnosis of IBD to A was 4 years, and A was diagnosed within 5 years after onset of IBD in 11 patients. Thirteen of the patients had suppurative complications; 12 had extraintestinal manifestations. Sixteen of the patients had been treated by bowel resection, 14 due to refractory IBD. Ten patients had been treated by renal transplantation. After 15 years of follow-up, the survival rate was 60%. Conclusions: Our findings strengthen the previous impression of an approximately 3-fold increased preponderance in males, with at least 10-fold increased frequency in CD compared with UC, and with a possible relationship to suppurative complications and extraintestinal manifestations, as well as an increased risk of having a bowel resection. The increased survival seems to be due to the introduction of renal transplantation.
BMJ case reports, 2011
Amyloidosis occurs as a result of the extracellular deposition of protein fibrils in organs and tissues, thus causing mild to severe pathophysiological changes. The gastrointestinal tract is a common site of amyloid deposition. While intestinal amyloidosis frequently results in polypoid lesions, ulcerations, nodules and petechial mucosal haemorrhage, tumour-like lesions are rarely developed and infrequently diagnosed before the resection because of the difficulty in differentiating them from colon cancer. The authors herein reported a case of intestinal amyloid A amyloidosis with a complication of a tumour-like lesion endoscopically resembling a malignant lesion, which was completely diminished after 1 month of observation with bowel rest. Such conservative treatment is a feasible option to cure intestinal tumour-like lesions in patients with intestinal amyloidosis when no neoplastic change is histologically detected, possibly decreasing the need for surgery of the fragile mucosa.
IOSR Journals , 2019
Amyloidosis of the Gastrointestinal tract with biopsy proven disease is rare. We present the clinical and histopathological features of localised intestinal amyloidosis with a rare case report. The patient had nonspecific gastrointestinal symptoms including haematochezia. Prior to treatment, the patient was suspected of having colo-colic intussusception on the basis of CT scan findings. The patient was treated with right hemicolectomy for caecal mass. The postoperative pathological diagnosis determined the lesion to be deposition of amyloid material with no evidence of malignancy. It was confirmed on congo red staining. Localised gastrointestinal amyloidosis is rare in incidence, but it should be considered in differential diagnosis of gastrointestinal tumours and confirmation can be done on biopsy. Although the condition is benign, there is a tendency of recurrence as suggested by literature.
Revista Espanola De Enfermedades Digestivas, 2022
Journal of Crohn's and Colitis, 2016
Background and Aims: Amyloidosis is a rare complication of inflammatory bowel disease [IBD]; its low prevalence has hindered both descriptive and therapeutic studies. The aim of this study was to estimate the prevalence of amyloidosis in IBD and the risk factors associated with this complication. Methods: This paper presents an observational study, followed by a systematic review of the epidemiological and clinical characteristics of the disease and a review of the diagnostic and therapeutic options. Results: The prevalence of amyloidosis among IBD patients is 0.53% (95% confidence interval [CI]: 0.32-0.75), although epidemiological data suggest that it may be under-diagnosed. The phenotype most frequently associated with amyloidosis is males with aggressive and extensive Crohn's disease, fistulising behaviour, perianal disease, and extra-intestinal complications, with the development of proteinuria and renal failure. Conclusions: Identifying risk factors of amyloidosis in IBD patients and screening for proteinuric renal dysfunction are useful to improve diagnostic accuracy. Referral of biopsies to a tertiary centre should also be considered, to improve diagnostic accuracy. Although there is no reliable evidence on the effectiveness of treatment, it seems reasonable to treat the underlying disease with potent immunosuppression to minimise inflammatory activity, thereby switching off amyloidogenesis.
Annals of Medical Research, 2019
Systemic amyloidosis is a rare disease characterized by extracellular accumulation of amyloid protein in one or more organs. In patients with systemic amyloidosis, the most frequently affected organs are kidney and heart, followed by the nervous system, soft tissues, and lungs. Small bowel and liver involvement are also frequent in systemic amyloidosis. Gastrointestinal (GI) findings are common, and the degree of organ involvement determines the symptoms. Patients usually have nonspecific findings such as abdominal pain, nausea, diarrhea, and dysphagia, which may delay the appropriate diagnosis. Liver involvement occurs in the majority of patients, but the symptoms typically do not happen unless a marked hepatic amyloid deposition occurs. Diagnosis is by tissue biopsy. Treatment and prognosis depend on the underlying disease. GI system involvement is a sign of poor prognosis. In this case series, five patients who were diagnosed with gastrointestinal system amyloidosis in our clinic are presented.
The Egyptian Journal of Internal Medicine
Amyloidosis is a rare condition where fibrillar proteins and abnormal, soluble peptides accumulate throughout the body’s organs. Gastrointestinal symptoms secondary to amyloid deposition vary widely and may be confused with other common small intestine diseases, making the diagnosis challenging. Our case is a 63-year-old male with a past medical history of smoking who showed up in the ED with 5 months of diffuse abdominal pain referred to the back. Pelvis-abdominal ultrasound showed bilateral acute pyelonephritis. A colonoscopy revealed large multiple ileal ulcers about 10 cm from the ileocecal valve with a wide base. Pathology biopsies revealed ileal amyloidosis and chronic ileitis with superficial erosions. The patient has been diagnosed with primary localized ileal AL amyloidosis. The patient has finally been referred for surgical resection. We want to raise awareness of ileal amyloidosis and emphasize the importance of considering uncommon etiologies of small intestine pathology...
Annals of Gastroenterology, 2017
Background Secondary systemic amyloidosis (SSA) is a rare but severe complication of inflammatory bowel disease (IBD). We aimed to evaluate the clinical characteristics, predictors of complications, and in-hospital mortality of patients with Crohn's disease (CD) and Ulcerative colitis (UC) who develop SSA. Methods Using the National Inpatient Sample, we identified patients hospitalized for IBD and SSA between 2004 and 2012. Using multivariate logistic regression, patients with CD were compared with those with UC regarding the presence or absence of SSA. IBD patients without SSA were matched in a 2:1 ratio with those with SSA using propensity matching. We analyzed the hospitalization trends of SSA in CD and UC patients using Pearson's χ 2 test. Analyses were performed using SAS version 9.3. Results Among the 302,548 patients with CD and 174,057 patients with UC hospitalized between 2004 and 2012, we identified 47 (0.02%) and 36 (0.02%) cases of SSA, respectively. We noted rising annual hospitalization trends for both CD and UC patients with or without SSA. In-hospital mortality was significantly higher for both the UC+SSA group (16.7% vs. 2.1%, P<0.0001) and the CD+SSA group (6.4% vs. 1.0%, P=0.0001) before propensity matching. However, this difference was not seen for either UC+SSA (17.1% vs. 7.1%, P=0.11) or CD+SSA (6.8% vs. 2.3%, P=0.20) after matching. Conclusions SSA rarely affects IBD patients, but when it does, it is associated with increased rates of infection, severe sepsis, and multi-organ system involvement. Despite this, SSA does not affect in-hospital mortality in IBD patients. Further studies are needed to explore this association.
Digestive Diseases and Sciences
Introduction Amyloidosis is an uncommon disease caused by the deposition of amyloid fibrils in tissues. This disease does not usually require surgical intervention, which could be warranted in the presence of complications such as bleeding, obstruction, or perforation. We present a case of primary amyloidosis of the colon in a patient affected by polymyositis who underwent Hartmann's procedure after a spontaneous colonic perforation. After 2 months of well-being, the patient underwent two consecutive surgical procedures for stenosis of the ostomy orifice. Areas Covered A review of the literature has been performed, gathering case reports highlighting the distribution of this disease by age, gender, location, and treatment when available. Expert Commentary Gastrointestinal amyloid disease is a rare condition, and it could be considered among the rare causes of intestinal perforation. Timely surgical management is often necessary.
Journal of Crohn's and Colitis, 2010
Background: Systemic amyloidosis is a rare but life-threatening complication of inflammatory bowel disease (IBD), most cases being reported among Crohn's disease (CD) patients. The only two available retrospective studies showed a prevalence ranging from 0.9% to 3% among CD patients. Aims: To evaluate the prevalence of secondary systemic amyloidosis in a large IBD cohort of a referral centre, and to describe its clinical characteristics and outcome. Methods: Patients diagnosed with amyloidosis were identified among 1006 IBD patients included in the IBD database of our centre, and their medical records were carefully reviewed. Results: Among a total of 1006 IBD patients, 5 cases of amyloidosis were identified, all of them with CD, resulting in a prevalence of 0.5% for IBD and 1% for CD. Two patients died after developing renal failure. Two patients were treated with anti-TNF agents, showing a clinical improvement of their amyloidosis. Conclusions: Secondary amyloidosis occurs mainly in long-lasting, complicated, Crohn's disease and seems to be as prevalent among IBD patients as previously reported.
World Journal of Gastroenterology, 2010
The involvement of the small bowel in systemic forms of amyloidosis may be diffuse or very rarely focal. Some cases of focal amyloidomas of the duodenum and jejunum without extraintestinal manifestations have been reported. The focal amyloidomas consisted of extensive amyloid infiltration of the entire intestinal wall thickness. Radiological barium studies, ultrasound and computed tomography (CT) patterns of diffuse small bowel amyloidosis have been described: the signs are non-specific and may include small-bowel dilatation, symmetric bowel wall thickening, mesenteric infiltration, and mesenteric adenopathy. No data are available about the positron emission tomography (PET)/CT and magnetic resonance imaging (MRI) patterns of intestinal amyloidosis. We report two cases of small bowel amyloidosis: the former characterized by focal deposition of amyloid proteins exclusively within blood vessel walls of the terminal ileum, the latter characterized by diffuse intestinal involvement observed on MRI and PET/CT studies.
The American Journal of Gastroenterology, 2000
patients without cirrhosis (median, 3.95 ng/ml; range, 3.38 -7.01 ng/ml), or with cirrhosis (median, 6.08 ng/ml; range, 5.13-8.91 ng/ml). The highest levels of sFas were found among PSC patients (median, 11.62 ng/ml; range, 4.55-17.69 ng/ml). sFasL was never detected in patients or controls, except for one PBC patient (0.359 ng/ml at baseline). We could not find any correlation between sFas baseline levels and other biological parameters (blood levels of hyaluronic acid, alkaline phosphatase, albumin, IgG and IgM, prothrombin time, and platelet counts) or histological stage. Soluble Fas levels could not predict the response to therapy neither, because they were not different between patients with complete response to UDCA therapy, defined by normalization of liver enzymes, and those who did not respond. Nevertheless, a slight, albeit significant, decrease in sFas levels was observed after therapy, evaluated for the 19 patients with a second serum available : median sFas: 5.46 ng/ml (range, 1.63-17.56 ng/ml) at baseline versus 4.71 ng/ml (range, 2.10 -8.62 ng/ml) after treatment (p ϭ 0.036). Again, no correlations were found between the decrease in sFas levels and the response to therapy.
Gastrointestinal Endoscopy, 2004
Amyloidosis is characterized by the deposition of amyloid proteins in various tissues and organs. 1 Although GI involvement is common, clinical manifestations are highly variable. 2 Although it usually does not cause symptoms, GI involvement may manifest as malabsorption, motility disorders, pseudotumor, intestinal perforation, and GI bleeding. 2-13 Rarely, GI bleeding is massive and can be fatal. 3-10 However, the diagnosis of GI amyloidosis is difficult because of the variable clinical manifestations and the nonspecific nature of endoscopic findings. Reported here is the case of a 51-year-old man with GI amyloidosis that manifested as massive bleeding from the small bowel and was controlled at surgery with the aid of intra-operative enteroscopy. CASE REPORT A 51-year-old man was referred with a 4-hour history of massive hematochezia. The patient had developed hypovolemic shock and received blood transfusions at another hospital. He had been in good health until 4 months earlier when he experienced 3 episodes of small amounts of hematochezia. At that time, colonoscopy at his primary hospital revealed no apparent abnormality except for an cecal polyp that was removed by polypectomy. The patient also had noted a recent 10-kg weight loss, anorexia, and mild nausea. He denied other symptoms such as abdominal pain, diarrhea, constipation, malaise, low back pain, and fever. He did not smoke tobacco or drink alcohol. There was no history of tuberculosis, rheumatoid arthritis, hepatitis, diabetes mellitus, or collagen-vascular disease. His family history was non-contributory. At admission, the patient looked pale, poorly nourished, and in acute distress. Blood pressure was 120/80 mm Hg and pulse rate 100 beats per minute. Examination was unremarkable; the abdomen was soft, non-tender, and without palpable mass or hepatosplenomegaly. Laboratory data at admission included the following: Hb 8.5 g/dL (normal: 13-17 g/dL), serum total protein 6.5 g/dL (6.0-8.0 g/
Open Journal of Hematology, 2014
Introduction: Primary systemic amyloidosis is the most common form of systemic amyloidosis. Clinical presentation commonly involves organs such as the kidney and heart. We report on a patient with systemic amyloidosis presenting as intractable diarrhoea. Numerous investigations had to be done before the diagnosis could be made highlighting the challenge in making a diagnosis due to the slow progression of the disease. This report is to increase awareness among physicians of this diagnosis and to emphasise the importance of identifying patients quickly. Case Presentation: A 63 year old male was admitted with a six months history of intractable, watery diarrhoea, anorexia and progressive renal failure. He had been investigated for proteinuria and deranged renal function prior to admission but no therapy was suggested and the diagnosis at that time was inconclusive. Extensive laboratory and radiological investigations were done. The diagnosis of systemic amyloidosis was made on serum free light chains which showed excess lambda chains and a terminal iliac and colonic biopsy which revealed eosinophilic thickening of the blood vessels with positive Congo red stain. Unfortunately the patient died prior to definitive management for the amyloidosis. Conclusion: This case emphasises the importance of early recognition of systemic amyloidosis so that management can be instituted.
Summary. Inflammatory Bowel Disease (IBD), which includes both Crohn’s Disease (CD) and Ulcerative Colitis (UC), is a chronic idiopathic inflammatory disorder affecting the gastrointestinal tract. Extraintestinal manifestations (EIMs) are common in patients with IBD, and occur in 6%-47% of patients with CD or UC. EIMs can involve organs other than the gastrointestinal tract such as skin, eyes, joints, biliary tract, and kidneys. Renal and urinary involvement particularly occurs in 4-23% of patients with IBD. Among the renal complications of IBD, secondary amyloidosis (AA-type, AAA) is a rare but serious complication. Renal amyloidosis has been proven to be the most common lethal manifestation of IBD-associated amyloidosis, since renal involvement rapidly leads to end-stage renal failure. A few studies suggest that AAA is more prevalent in CD than in UC, mainly occurring in male patients with an extensive, long-lasting, and penetrating disease pattern. The therapeutic approaches of IBD-associated AAA are based both on control of the chronic inflammatory process that causes the production and storage of serum amyloid A (SAA), which is a precursor of the amyloid, as well as on destabilizing amyloid fibrils so that they can no longer maintain their β-pleated sheet configuration; however, in patients with end-stage renal disease, the only therapeutic options still available are hemodyalisis and renal transplantation. Whether effective treatment exists for AAA remains controversial.
2003
Since amyloidosis was first described in 1886, an enormous amount of literature has been published. In most patients with systemic amyloidosis, the entire gastrointestinal tract is involved. The clinical manifestations vary from asymptomatic, impaired motor activity, bleeding, perforation to death. Patel et al first reported a case of small bowel diverticula caused by amyloidosis in 1993 (1). Intestinal perforation is a very rare complication of amyloidosis and previous reports have suggested a poor prognosis (2-6). CASE REPORT A 91-year-old black female was admitted with the chief complaint of palpitations. She had no chest pain, no shortness of breath, no nausea or vomiting, no diaphoresis, and no previous episodes of this ever happening. The patient had some weakness for the last two to three weeks, malaise, and fatigue that had progressively gotten worse. She had questionable hypertension, and she was taken off of blood pressure medication seven years ago. She had a laparotomy for possible bowel obstruction 60 years ago. On physical examination she was a thin black female in no apparent distress. Respiratory and cardiovascular examinations were normal; the abdomen was soft with no tenderness, and the bowel sounds were normal. Rectal examination revealed hemepositive stools. Laboratory studies revealed the following values: hemoglobin, 5.1 g/dl, hematocrit 17.8%; normal BMP except for a potassium of 3.1, total protein 6.1 g/dl, albumin 3.2 g/dl, serum iron 6 µg/dl, total iron binding capacity 371 µg/dl, and ferritin 8.6 ng/ml. Results of the urinalysis showed no Manuscript

Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
 Shiva Kumar R Mukkamalla
Shiva Kumar R Mukkamalla