CMR evaluation in patients with high grade ventricular arrhythmias
2009, Journal of Cardiovascular Magnetic Resonance

Sign up for access to the world's latest research
Abstract
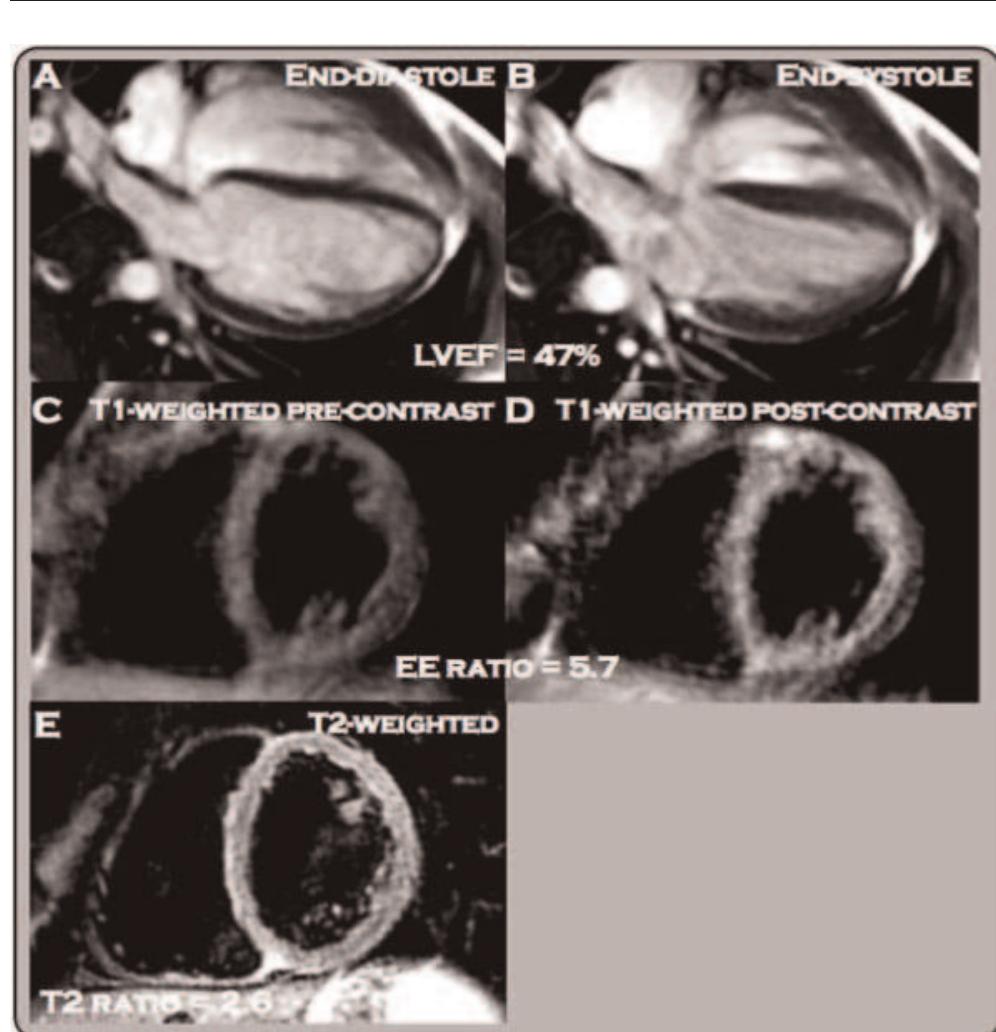
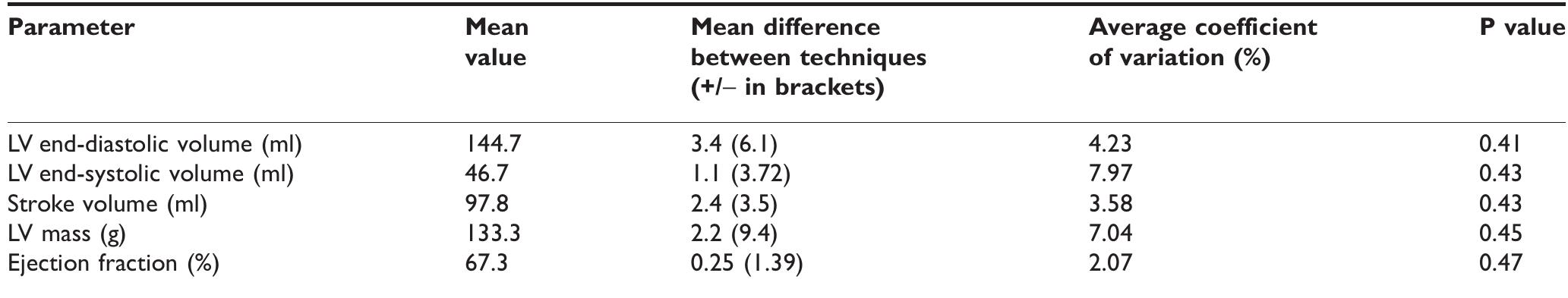
ABSTRACT PURPOSE To assess by cardiac-MR the prevalence of myocardial morphologic and/or functional alterations in arrhythmic patients. METHOD AND MATERIALS We examined 43 patients with non ischemic ventricular arrhythmias. Premature ventricular complexes had left bundle branch block morphology(LBBB) in 29 cases, in 7 a right bundle branch block contour(RBBB) and 7 had polymorphic patterns(PV). US was negative in 78.4% of patients, while CMR was negative in only 13% of patients. Studies were performed on a 1.5 MR scanner with Cine sequences (FIESTA), bb-FSE and IR-prep FGRE 15 minutes after injection of 0,2 mmol/Kg of Gd-DTPA. RESULTS CMR found a high prevalence of morphological, signal intensity and functional myocardial abnormalities. RV dilatation was found in 85% of patients with PV arrhytmias, 48.3% of patients with LBBB morphology, 12.5% of patients with RBBB morphology. LV dilatation was present in 28.6%, 25% and 24.1 % of patients with LBBB, PV and RBBB type arrhytmias respectively. RV wall motion abnormalities were identified in 50% and 36.7 % of patients with PV and LBBB pattern respectively; LV wall motion abnormalities in 25% and 10.3% of patients with PV and LBBB pattern respectively. Free wall RV signal/thickness abnormalities were found in 23,3% of patients(18.6% with LBBB pattern and 4.7 with PV pattern); LV signal abnormalities were found in 11.6% of patients(9.3% with LBBB pattern and 2.3% with PV pattern). Seven patients underwent myocardial biopsy: 5 were positive for myocarditis, 1 was positive for ARVD, one had a negative biopsy. CONCLUSION In patients with primary ventricular arrhythmias CMR documented high prevalence (87%) of morphological, signal intensity and wall motion abnormalities even with negative echocardiogram. CLINICAL RELEVANCE/APPLICATION CMR sholud be considered first choice technique in patients with high grade non ischemic ventricular arrythmias, to select candidates for endomyocardial byopsies and to guide the site of the byopsy.



![Table | (abstract O4) Imaging parameters edematous myocardium (T1/T2 = 1119/101.8 ms) [2]. Phantom T| and T2 values were verified using a standard spin echo sequence. as and T2 values were verified using a standard spin echo sequence. In-vivo: T2 Maps were acquired in 9 healthy subjects to determine the normal range of T2 values. Three short-axis and two long-axis views were imaged during breath hold (duration ~5 HB) and in free breathing using navigator gating. In 5 subjects, four averages were acquired with navigator gating to test the benefits of increased SNR. Average T2 values were calculated in 16 myocardial segments using both methods and compared. Measurements were pooled to obtain global mean and standard deviation to investigate inter-subject and inter-segment variability.](https://figures.academia-assets.com/42006955/table_002.jpg)












![Left: CNR (mean + stdev) at different TI values in PS-DIR signed images (red) and in DIR magnitude images at TI* (green). Right: Wall thickness at different Tl using PS-DIR images (red) and using DIR images at TI*. Note the agreement with the measurements using TI*. Dual-slice single breath-hold PS-DIR Coronary vessel wall black-blook imaging Experiments: Anatomical slices perpendicular to the proximal part of the right coronary artery (RCA) at end-systole were planned similar to a previously published methodology [7]. First, serial single-slice multi-phase PS-DIR images were acquired with incremental Tl ranging from 50 ms—500 ms in |5 healthy adult](https://figures.academia-assets.com/42006955/figure_015.jpg)










































![Table | (abstract O47) Comparison between EPI-FLASH and TrueFISP with identical resolution and imaging time Volunteer imaging: 7 volunteers were scanned on a 1.5 T Espree scanner (Siemens Medical Solutions). Scan parameters were: TR = 11.3, TE = 4.27, flip angle = 25, 66 lines per heartbeat in a window of 124 ms, acquired k-space lines = 132, readout bandwidth = 977 Hz/pixel, Tl = 300 ms, matrix: 256 x 189 x 60, interpolated voxel size: 0.5 x 0.55 x | mm?. 0.2 mmol/kg body weight of Gd-DTPA was injected at 0.5 cc/sec [5]. The total imaging time for the whole-heart scan was](https://figures.academia-assets.com/42006955/table_012.jpg)




![Arrows identify patterns of MDE. a) transmural; b) subendocardial; c) EFE; d) subepicardial/intramural. Results: Of the 85 subjects included (65% male; median age at Fontan 4.5 [2.0, | 1.2] years; mean age at CMR 23.1 + | 1.2 years), 21 (25%) had positive MDE in the ventricular myocardium. MDE was seen in the following locations: dominant ventricle free wall (n = 13, 62%), secondary ventricle free wall (n = 9, 43%), septal insertion (n = 5, 24%), ventricular septum (n = 3, 14%), apex (n = 2, 10%), previous surgical sites (n = 2, 10%), and papillary muscle (n = 2, 10%). MDE was seen in the following patterns: transmural lesion](https://figures.academia-assets.com/42006955/figure_056.jpg)

![The T2 maps of a normal (a) and a DMD subject (b) showing the left ventricle in the short axis view. Values are mean + SD, median [25%, 75%], or n (%); ‘Student t test, *Mann-Whitney U test, *Fisher exact test, *Chi-squared test of independence.](https://figures.academia-assets.com/42006955/figure_057.jpg)








![Methods: Fifty elderly subjects [mean age = 65 (+ 8), 16/ 50 = 32% women] with at least one major cardiovascular risk factor (smoking, diabetes, hypertension, hyperlipidemia) under- went MRI (1.5 T Siemens Sonata) for abdominal and peri-aortic adipose tissue quantification and aortic atherosclerosis asses-](https://figures.academia-assets.com/42006955/figure_067.jpg)






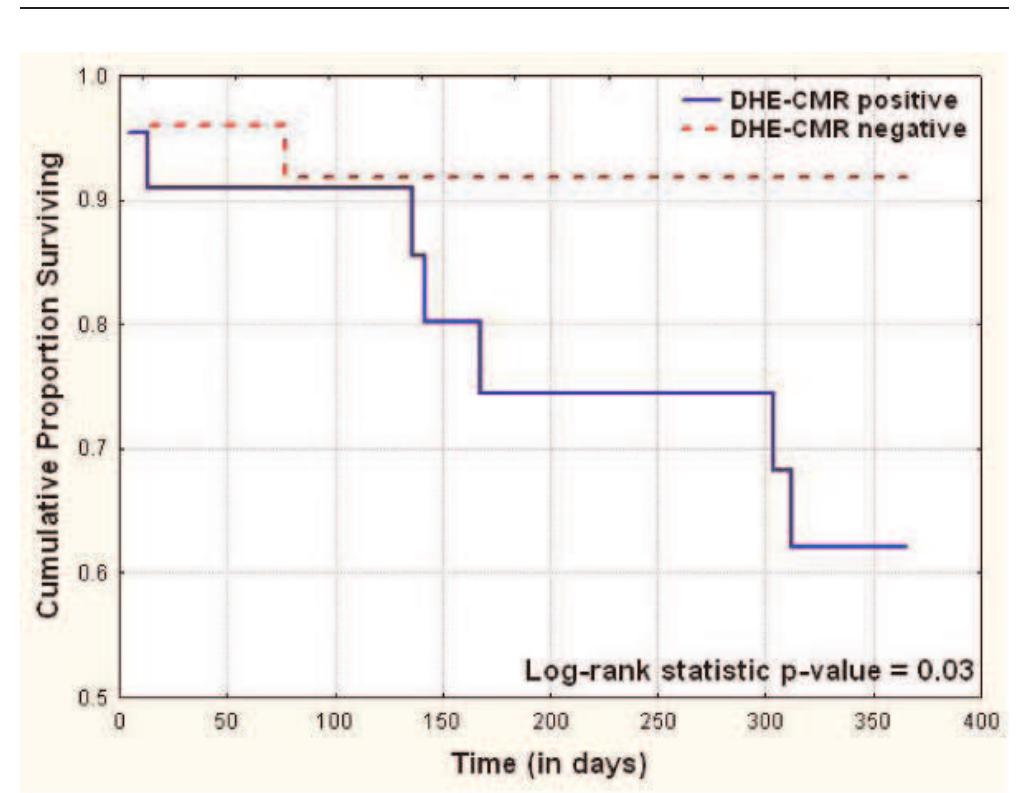
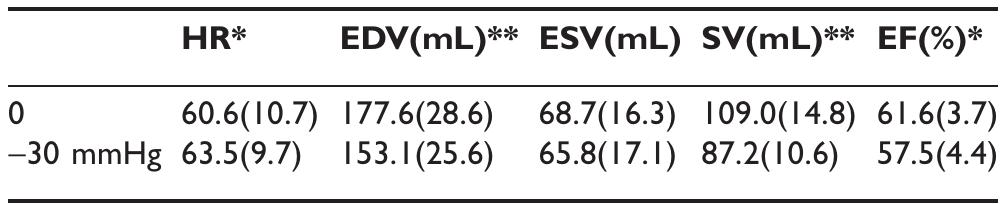
![appearance, E/A ratio, E/E’ ratio, stage of diastology, deceleration time (msec) and myocardial performance index [(isovolumic contraction time + isovolumic relaxation time)/ejection time]. DHE-MR images were obtained in standard long and short axis orientations (covering the entire LV), after injection of Gadolinium dimenglumine using an inversion recovery spoiled gradient echo sequence: TE 4 msec, TR 8 msec, flip angle 30°, bandwidth 140 Hz/pixel, 23 k-space lines acquired every other RR-interval, field of view (varied from 228-330 in the x-direction and 260-330 in the y-direction) and matrix size (varied from 140-180 in the x-direction and 256 in the y-direction). CMR was considered positive in the presence of DHE of entire sub- endocardium with extension into the neighboring myocardium.](https://figures.academia-assets.com/42006955/figure_072.jpg)







































































![Table | (abstract P24) Acquisition parameters for Tlw-SPACE and ce-MRA and bulk head motion during the long 3D acquisition time. Respiratory movement artefact is controversial [4], but Boussel [5] demonstrated its detrimental effect on carotid wall imaging, using real-time transaxial cines. However, during quiet supine respiration, breathing is predominantly diaphragmatic resulting in the greatest carotid movement in the head-foot direction. We used a novel high temporal resolution interleaved approach to study carotid artery movement in all directions, over the typical 3D scan duration, for a true representation of the potential problem for 3D imaging. Siemens, Erlangen) using two body matrix coils for the abdominal/pelvic area and a peripheral coil for thighs and lower legs. The imaging protocol included localizers, coronal acquisition of abdominal aorta and SFA using TIlw-SPACE, followed by ce-MRA covering the abdomen, thighs and the lower legs.](https://figures.academia-assets.com/42006955/table_029.jpg)

















































![Results: The dual cardiac phase whole heart scan was applied successfully in all patients. An example of each coronary segment is shown in figure |. The vessel length, diameter, sharpness and consensus score for each segment during systole and diastole are shown in Table |. Bland Altman plots of the systolic versus diastolic data from each coronary segment are shown in figure 2. No statistically difference was found comparing vessel length, diameter, sharpness for all vessels between systole and diastole. Moreover, no statistically differ- ence was found in image quality. Although, there was no difference for the mean vessel length, diameter, and sharpness, it was found that on a patient level, those parameters and image quality showed differences either favoring systolic or diastolic image acquisition for different coronary segments within the same patient. SEIS YSLONE GLI TERESI SLO Pildse HT COMPUTICLIOTT WIC LI WHOL heart approach allows retrospectively selection of the best image phase for coronary artery visualization without any scan time penalty. Methods: Eight children (age = 6.38 + 4.27, height = 116.57 + 30.77, weight = 23.57 + 14.25, Heart-rate = 85.02 + 8.59) with CHD were scanned under general anesthesia on a 1.5 T MR system (Achieva, Philips Healthcare). The cardiac rest period for end-systole and mid-diastole was determined from a 2D SSFP cine scan with high temporal resolution (TR/TE = 3.1/1.6 ms, flip angle 60°, slice thickness 6 mm, 60 to 80 cardiac phases). A previously developed free-breathing navigator gated 3D SSFP dual cardiac phase sequence [I] was then applied in sagittal orientation for imaging of the whole heart including the coronary arteries and great vessels (TR/TE = 3.4/1.7 ms, flip angle 90°, 60-120 slice, isotropic resolution of I-I.5 mm?, temporal resolution of 60 — 75 ms, Sense of 2 in AP direction). Data was obtained during end-systole and mid-diastole and the acquisition window of the 3D scan was adapted accordingly to the shortest rest period. Images were then reformatted along the major axes of the left and right coronary artery for both cardiac phases. Vessel length, diameter and sharpness of the visualized coronary arteries (RCA, LM, LAD, LCx) were measured using the “SoapBubble” software. Image quality was assessed by two independent observers. Statistical analysis and Bland Altman plots were used to compare the different data sets.](https://figures.academia-assets.com/42006955/figure_179.jpg)




![Final myocardium contours on 4 different patients. Then the delineation of the myocardial contours is performed by alternating automatic deformation of a geometrical template and computation of a binary map of the enhanced areas. The template is ribbon-shaped with a variable width, its position is updated depending on image gray values. The map is a 2D binary image showing enhanced areas, it is updated by thresholding the image gray values in a region of interest centered on the endocardium, in order to include sub-endocardial scars. The segmentation is performed as follows: (1) automatic delineation of myocardial contours on short-axis LECMR slices [2],](https://figures.academia-assets.com/42006955/figure_182.jpg)









![First-pass perfusion image before (left) and after (right) KLT filtering. KLT filter provides marked noise suppression without loss of contrast between normally and abnormally perfused regions. Methods: Ten consecutive first-pass perfusion datasets inter- preted positive for ischemia or infarction were processed and analyzed retrospectively. All images were acquired using GRE-EPI with TSENSE acceleration rate 2 on a 1.5 T MR system (MAGNETOM Avanto, Siemens Healthcare, Germany). For each subject, all slices showing clinically interpreted perfusion defect were included in the analysis. Non-rigid body registration [3] was first performed on each series to allow for semi- quantitative analysis of signal enhancement, and to improve the](https://figures.academia-assets.com/42006955/figure_190.jpg)











![64-year-old female with mean PAP = 51 mmHg demonstrates hypertro- phy of SMT (septomarginal trabecula), white arrow, in a dilated right ventricle. Introduction: In the right ventricle (RV), the septomarginal trabecula (SMT) arises as a muscular band originating from the interventricular septum (IVS) at the lower segment of the crista supraventricularis. It forms a functional unit with the moderator band, which attaches to the lateral free wall of the RV [I, 2]. Strategically situated between the RV inflow and outflow tracts, the whole unit serves to help emptying blood into the pulmonary trunk during systole. Thus, it should be anticipated that the SMT may undergo changes in RV hypertrophy secondary to chronic pulmonary hypertension.](https://figures.academia-assets.com/42006955/figure_203.jpg)
![Figure 3 (abstract P91) Methods: Imaging was performed in two centers; one using 3 T and the other using |.5 T MR systems. 33 catheter proven PAH patients (mean age = 61.4 + 12.1 years and mPAP = 45.9 + 12.4 mmHg) were enrolled in the study [Idiopathic pulmonary arterial hypertension (IPAH) = 21 and Scleroderma (SSc) = 12 patients]. Similarly, 9 healthy volunteers (mean age = 45.56 + 8.6 years) were included in the study for comparison. Short axis cine images were acquired using fast gradient echo technique. End diastolic frames were analyzed using MASS 6.2.1 software (Medis, the Netherlands). Starting from the basal slices, the SMT was identified in patients and controls as the most anterior trabeculation arising from the IVS below the outflow tract level. Two independent observers manually contoured and traced the SMT from its origin towards the apex where the moderator](https://figures.academia-assets.com/42006955/figure_204.jpg)






















![Methods: We retrospectively reviewed 7] consecutive cardiac magnetic resonance (CMR) studies for BPA size and PCMR data. We also reviewed |3 consecutive pts who underwent both CMR and catheterization.](https://figures.academia-assets.com/42006955/figure_225.jpg)






















![Examples of T2* curve fitting using both truncation and offset models. Left: In vivo scan data; Right: Ex vivo heart data. Methods: A 23-year-old Thai female thalassemia majorpatient with longstanding cardiac and liver iron overload was studied. The patient underwent MRI scan using the bright blood T2* sequence [2] (twice for reproducibility) in Bangkok on a 1.5 T clinical scanner (GE Signa), again in London 9 days later on a 1.5 T one (Siemens Sonata), using the same sequence. The patient was also scanned using the black blood T2* sequence [4]. The patient died two weeks later. With full ethical approval, the donated heart was formalin fixed before being sliced axially. A](https://figures.academia-assets.com/42006955/figure_246.jpg)








































![Table | (abstract P167) Basal slice mean peak tangential strain values and standard deviation for three confirmed ARVC cases, six suspected cases, and four normal volunteers for the LV and RV segments of abnormal strain and motion, which occur largely in the region of the RV insertion points and the LV inferior and anterior septum. Abnormal RV strain patterns were evident in 2 out of the 3 confirmed, and 3 out of the 6 suspected cases. The other confirmed case had a dilated RV but the strain pattern appeared normal. Table | presents regional peak tangential strains for the basal slice averaged for each group. A confidence measure for Ett was calculated based on the signal-to-noise ratio (SNR) of the magnitude images. Only Ett strain values with confidence greater than 0.5 (normalized to max confidence in entire heart) were used to compute regional peak Ett strain. More than half of the data points in the diaphragmatic RV had to be discarded because of low SNR. Both confirmed and suspected ARVC cases have low peak strain values in the inferior and anterior septum and the RV free wall. Peak Ett is significantly less in ARVC and suspected ARVC cases compared to normals in the anterior septum (p < 0.005 and p < 0.05, respectively, student t-test). over two breath holds per slice. Imaging parameters include: FOV = 400 mn, slice thickness = 7.0 mm, TR = 24 ms, FOV phase = 62.5%, ETL = 9, segments = 18, cardiac phases = |0- 16, and displacement encoding frequency = 0.1 cycles/mm. Epicardial and endocardial contours were manually drawn for both the LV and RV on all cardiac phases. Phase unwrapping and tissue tracking were performed [5], and motion trajectories were estimated using temporal fitting with 5“ order Polynomial functions. Lagrangian strain taken tangential to the midwall (Ett) was computed from both the left ventricle (LV) and RV motion trajectories [3].](https://figures.academia-assets.com/42006955/table_059.jpg)














































![Table | (abstract P216) Optimal imaging parameters for cardiac imaging with T2w-SPACE as acute myocarditis and acute myocardial infarction [2, 3]. 3D acquisitions can provide high resolution images of the whole heart, allowing arbitrary views of the organ, and reducing partial volume effect. Conventional 3D TSE improves SNR but not sampling efficiency or spatial resolution. We propose a novel TSE technique for T2w 3D imaging of the whole heart that provides higher spatial resolution and reduces scan time per slice compared to 2D DB-TSE.](https://figures.academia-assets.com/42006955/table_068.jpg)












































![2) Update of k-space should smoothly vary over time (as in KT- BLAST/SLAM) avoiding sudden transitions between k-space regions to result in smoother transition between frames. Introduction: Previously, we developed a sparsely distribute k-space-time sampling approach termed BRISK, Block Regional Interpolation Scheme for K-space [I]. This approach allowed a nominal acceleration factor of 4 with good quality and low artifact. Others have developed alternative k-space-time sampling schemes, such as KT-BLAST and SLAM [2, 3]. We note that even at high acceleration factors, KT-BLAST/SLAM allowed a smooth transition from frame to frame, while BRISK experienced ringing artifacts. From these considerations we isolated key features that contribute to a successful k-space-time sparse sampling scheme: |) Update of k-space should be rapid near the center and lower near the periphery (as in BRISK) to capture highly dynamic features.](https://figures.academia-assets.com/42006955/figure_361.jpg)































![Simulation of magnetization signal intensity regrowth curves of blood (TI = 300 ms), diffuse fibrosis (T] = 350 ms) and normal myocardium (TI = 380 ms), after a 180° pulse. Zoomed view shows the difference in null times between blood, diffusely fibrosed myocardium and normal myocardium (ATI, and ATI,). Sb; is the blood signal intensity when normal myocardium is nulled, and Sb» is the blood signal intensity when diffusely fibrosed myocardium in nulled.](https://figures.academia-assets.com/42006955/figure_389.jpg)





















Related papers
Journal of Cardiovascular Magnetic Resonance, 2011
Cite this article as: Weisser-Thomas J, Ferrari VA, Lakghomi A, Lickfett LM, Nickenig G, Schild HH, et al. Prevalence and clinical relevance of the morphological substrate of ventricular arrhythmias in patients without known cardiac conditions detected by cardiovascular MR. Br J Radiol 2014;87: 20140059. FULL PAPER Prevalence and clinical relevance of the morphological substrate of ventricular arrhythmias in patients without known cardiac conditions detected by cardiovascular MR 1
European Heart Journal, 1997
Journal of Nuclear Cardiology, 2019
2001
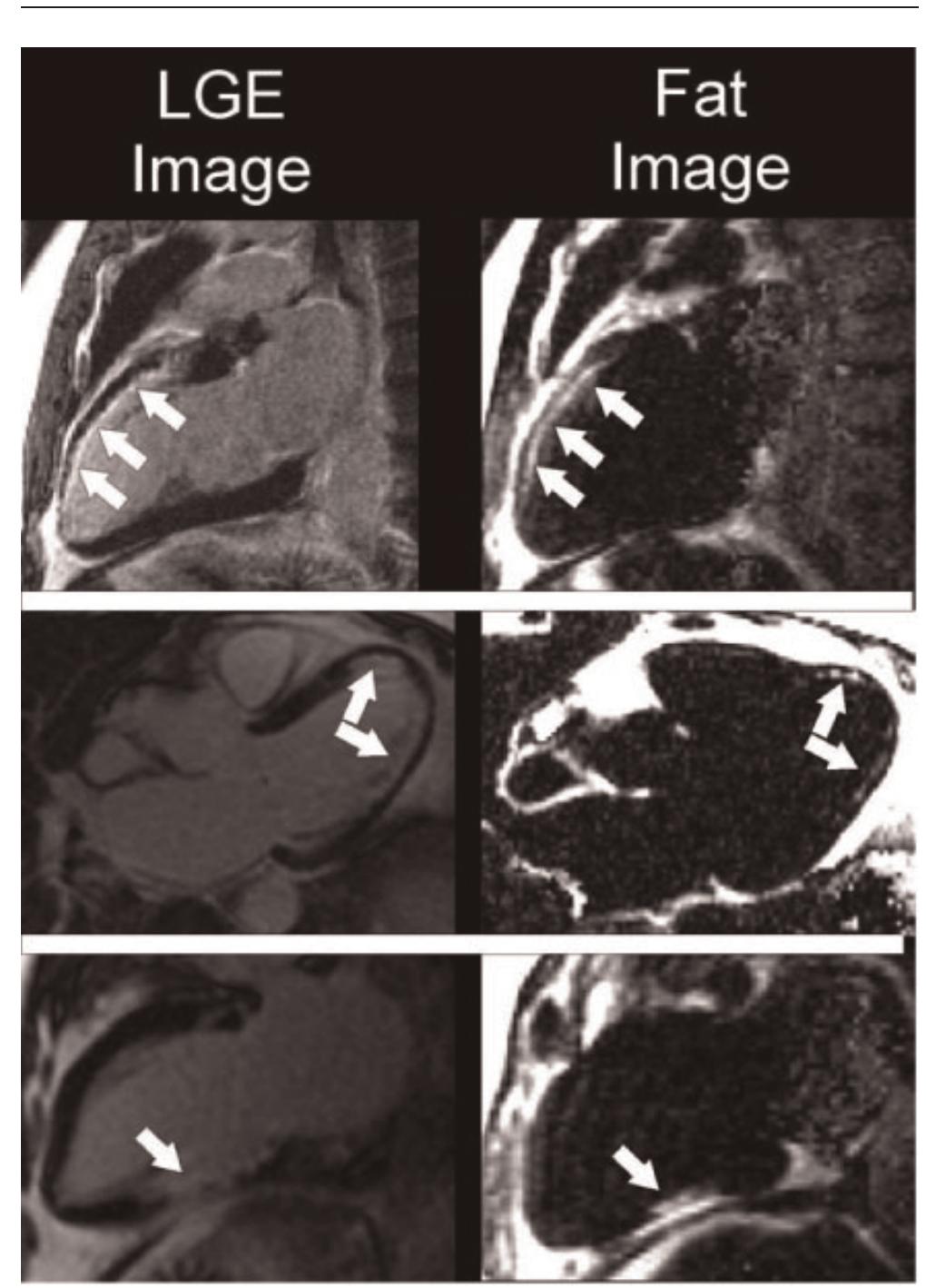
Summary Arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C) is among the major factors for mortality in young adults. Therefore, early diagnostics and institution of therapy, e.g. antiarrhythmics, radio frequency ablation, or implantable cardioverter/defibrillator, are unavoidable. Cardiac magnetic resonance imaging (MRI) is unique in the diagnosis of ARVD/C, since this non-invasive tool detects tissue-specific information with a simultaneous, direct measurement of the left- and right-ventricular function, regional wall motion abnormalities and morphology. A suitable T1 (spin-lattice relaxation time) sensitive MRI acquisition can differentiate pericardial, epicardial, and patchy or diffuse right ventricle lipid infiltration from the true myocardial tissue. We studied 31 patients with symptomatic ventricular arrhythmia with left bundle branch block morphology and a suspected diagnosis of ARVD/C. Only six out of 31 patients fulfilled the diagnostic criteria for ARVD/C. ...
2014
Background-Routine diagnostic work-up occasionally does not identify any abnormality among patients with monomorphic ventricular arrhythmias (VAs) of left ventricular (LV) origin. Aim of this study was to investigate the value of cardiac MRI (cMRI) for the diagnostic work-up and prognostication of these patients. Methods and Results-Forty-six consecutive patients (65% males; mean age, 44±15 years) with monomorphic VAs of LV origin and negative routine diagnostic work-up were included. Seventy-four consecutive patients (60% males; mean age, 40±17 years) with apparently idiopathic monomorphic VAs of right ventricular origin served as control group. Both groups underwent comprehensive cMRI study and were followed-up for a median of 14 months (25th-75th percentiles, 7-37 months). The outcome event was an arrhythmic composite end point of sudden cardiac death or nonfatal episode of ventricular fibrillation or sustained ventricular tachycardia requiring external cardioversion or appropriate implantable cardioverter defibrillator therapy. The 2 groups of patients did not differ in age (P=0.14) and sex (P=0.57). No significant difference was observed between patients with VAs of LV origin and VAs of right ventricular origin about biventricular volumes and systolic function. cMRI demonstrated myocardial structural abnormalities in 19 (41%) patients with VAs of LV origin versus 4 (5%) patients with VAs of right ventricular origin (P<0.001). The outcome event occurred in 9 patients; myocardial structural abnormalities on cMRI were significantly related to the outcome event (hazard ratio, 41.6; 95% confidence interval, 5.2-225.0; P<0.001).
Journal of the American College of Cardiology, 2011
Pacing and clinical electrophysiology : PACE, 2012
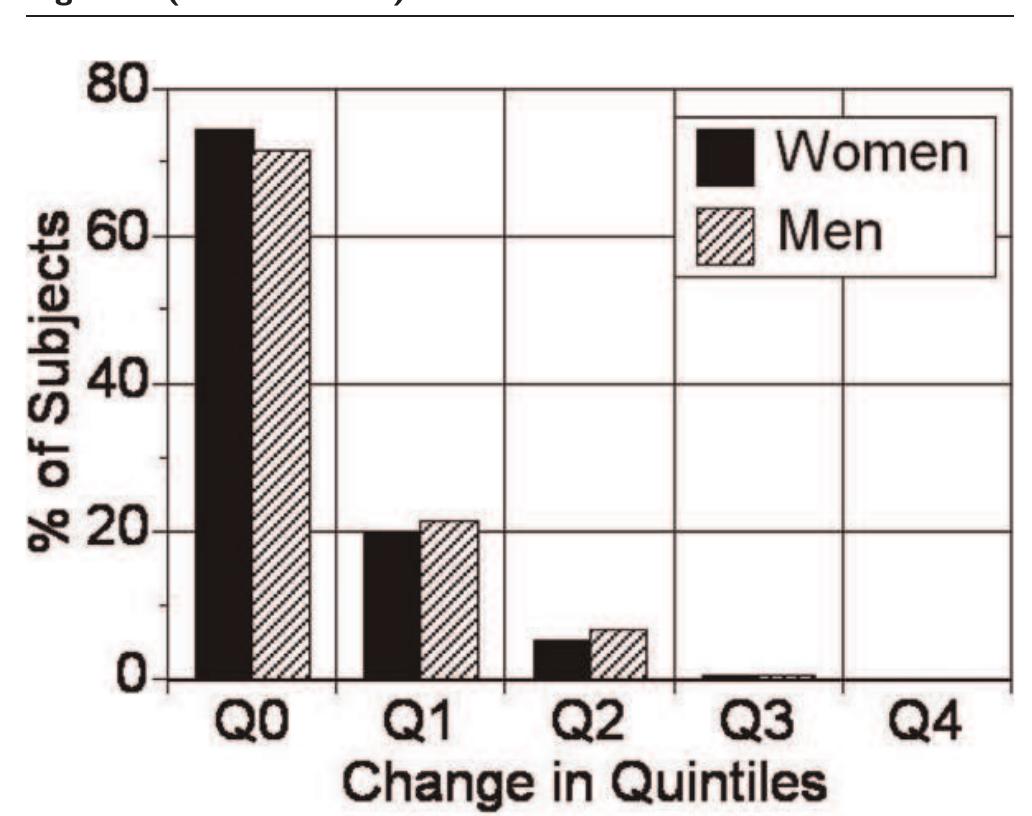
Background: Idiopathic ventricular arrhythmias in the form of monomorphic premature ventricular contractions (PVC) and/or ventricular tachycardia (VT) can cause tachycardia-induced cardiomyopathy (TICMP). The aim of this study was to determine the prevalence of late gadolinium enhancement (LGE) in patients with TICMP caused by idiopathic ventricular arrhythmias. Methods: The study population consisted of 298 consecutive patients (174 F/124 M; mean age 45 ± 17 years) with frequent PVCs and/or VT. TICMP was defined as left ventricular ejection fraction (LVEF) of ≤50% in the absence of any detectable underlying heart disease and improvement of LVEF ≥15% after effective treatment of index ventricular arrhythmia. Results: Twenty-seven (9.1%) patients found to have LVEF ≤50% and diagnosed as presumptive TICMP. Improvement in LVEF after effective treatment of index ventricular arrhythmia was observed in 22 of 27 patients (TICMP group; mean PVC burden of 30.8 ± 9.9%). LVEF did not improve i...
Tribology International
Journal of Cardiovascular Magnetic Resonance, 2009
Introduction: Prophylactic implantation of a cardioverter/ defibrillator (ICD) has been shown to reduce mortality in patients with chronic myocardial infarction (CMI) and an increased risk for life threatening ventricular arrhythmia (VA). The use of ICDs in this large patient population is still limited by high costs and possible adverse events including inappropriate discharges and progression of heart failure. VA is related to infarct size and seems to be related to infarct morphology. Contrast enhanced cardiovascular magnetic resonance imaging (ceCMR) can detect and quantify myocardial fibrosis in the setting of CMI and might therefore be a valuable tool for a more accurate risk stratification in this setting. Hypothesis: ceCMR can identify the subgroup developing VA in patients with prophylactic ICD implantation following MADIT criteria. Methods: We prospectively enrolled 52 patients (49 males, age 69 ± 10 years) with CMI and clinical indication for ICD therapy following MADIT criteria. Prior to implantation (36 ± 78 days) patients were investigated on a 1.5 T clinical scanner (Siemens Avanto © , Germany) to assess left ventricular function (LVEF), LV end-diastolic volume (LVEDV) and LV mass (sequence parameters: GRE SSFP, matrix 256 × 192, short axis stack; full LV coverage, no gap; slice thickness 6 mm). For quantitative assessment of infarct morphology late gadolinium enhancement (LGE) was performed including measurement of total and relative infarct mass (related to LV mass) and the degree of transmurality (DT) as defined by the percentage of transmurality in each scar. (sequence parameters: inversion recovery gradient echo; matrix 256 × 148, imaging 10 min after 0.2 μg/kg gadolinium DTPA; slice orientation equal to SSFP). MRI images were analysed using dedicated software (MASS © , Medis, Netherlands). LGE was defined as myocardial areas with signal intensity above the average plus 5 SD of the remote myocardium. After implantation, patients were followed up including ICD readout after 3 and than every 6 months for a mean of 945 ± 344 days. ICD data were evaluated by an experienced electrophysiologist. Primary endpoint was the occurrence of an appropriate discharge (DC), antitachycard pacing (ATP) or death from cardiac cause. Results: The endpoint occurred in 10 patients (3 DC, 6 ATP, 1 death). These patients had a higher relative infarct mass (28 ± 7% vs. 22 ± 11%, p = 0.03) as well as high degree of transmurality (64 ± 22% vs. 44 ± 25%, p = 0.05). Their LVEF (29 ± 8% vs. 30 ± 4%, p = 0.75), LV mass (148 ± 29 g vs. 154 ± 42 g, p = 0.60), LVEDV (270 ± 133 ml vs. 275 ± 83 ml, p = 0.90) or total infarct mass (43 ± 19 g vs. 37 ± 21 g, p = 0.43) were however not significant from the group with no events. In a cox proportional hazards regression model including LVEF, LVEDV, LV mass, DT and age, only degree of transmurality and relative infarct mass emerged as independent predictors of the primary end point (p = 0.009). Conclusion: In CMI-patients fulfilling MADIT criteria ceCMR could show that the extent and transmurality of myocardial scarring are independent predictors for life threatening ventricular arrhythmia or death. This additional information could lead to more precise risk stratification and might reduce adverse events and cost of ICD therapy in this patient population. Larger trials are needed to confirm this finding.
Diagnostics
Background: A routine diagnostic work-up does not identify structural abnormalities in a substantial proportion of patients with idiopathic ventricular arrhythmias (VAs). We investigated the added value of cardiac magnetic resonance (CMR) imaging in this group of patients. Methods: A single-centre prospective study was undertaken of 72 patients (mean age 46 ± 16 years; 53% females) with frequent premature ventricular contractions (PVCs ≥ 500/24 h) and/or non-sustained ventricular tachycardia (NSVT), an otherwise normal electrocardiogram, normal echocardiography and no coronary artery disease. Results: CMR provided an additional diagnostic yield in 54.2% of patients. The most prevalent diagnosis was previous myocarditis (23.6%) followed by possible PVC-related cardiomyopathy (20.8%), non-ischaemic cardiomyopathy (8.3%) and ischaemic heart disease (1.4%). The predictors of abnormal CMR findings were male gender, age and PVCs/NSVT non-outflow tract-related or with multiple morphologies...
Journal of Nuclear Cardiology, 2010
Journal of the American College of Cardiology, 2006
The American Journal of Cardiology, 1990
Cardiology, 2003
Background: Magnetic resonance (MR) imaging is frequently used to diagnose arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC/D). However, the reliability of various MR imaging features for diagnosing ARVC/D is unknown. The purpose of this study was to determine which morphologic MR imaging features have the greatest interobserver reliability for diagnosing ARVC/D. Methods: Forty-five sets of films of cardiac MR images were sent to 8 radiologists and 5 cardiologists with experience in this field. There were 7 cases of definite ARVC/D as defined by the Task Force criteria. Six cases were controls. The remaining 32 cases had MR imaging because of clinical suspicion of ARVC/D. Readers evaluated the images for the presence of (a) right ventricle (RV) enlargement, (b) RV abnormal morphology, (c) left ventricle enlargement, (d) presence of high T 1 signal (fat) in the myocardium, and (e) location of high T 1 signal (fat) on a Likert scale with formatted responses. Results: Readers indicated that the Task Force ARVC/D cases had significantly more (¯2 = 119.93, d.f. = 10, p ! 0.0001) RV chamber size enlargement (58%) than either the suspected ARVC/D (12%) or no ARVC/D (14%) cases. When readers reported the RV chamber size as enlarged they were significantly more likely to report the case as ARVC/D present (¯2 = 33.98, d.f. = 1, p ! 0.0001). When 154 Cardiology 2003;99:153-162 Bluemke et al.
International Journal of Cardiology, 2012
American Heart Journal, 2008
Background Prior reports describing magnetic resonance (MR) imaging abnormalities in arrhythmogenic right ventricular dysplasia (ARVD/C) were limited by nonuniform inclusion criteria. The aim of our study was to define the prevalence, sensitivity, and specificity of quantitative MR imaging findings in the probands of multidisciplinary study of right ventricular dysplasia.
Journal of Cardiovascular Magnetic Resonance, 2009
Introduction: Prophylactic implantation of a cardioverter/ defibrillator (ICD) has been shown to reduce mortality in patients with chronic myocardial infarction (CMI) and an increased risk for life threatening ventricular arrhythmia (VA). The use of ICDs in this large patient population is still limited by high costs and possible adverse events including inappropriate discharges and progression of heart failure. VA is related to infarct size and seems to be related to infarct morphology. Contrast enhanced cardiovascular magnetic resonance imaging (ceCMR) can detect and quantify myocardial fibrosis in the setting of CMI and might therefore be a valuable tool for a more accurate risk stratification in this setting. Hypothesis: ceCMR can identify the subgroup developing VA in patients with prophylactic ICD implantation following MADIT criteria. Methods: We prospectively enrolled 52 patients (49 males, age 69 ± 10 years) with CMI and clinical indication for ICD therapy following MADIT criteria. Prior to implantation (36 ± 78 days) patients were investigated on a 1.5 T clinical scanner (Siemens Avanto © , Germany) to assess left ventricular function (LVEF), LV end-diastolic volume (LVEDV) and LV mass (sequence parameters: GRE SSFP, matrix 256 × 192, short axis stack; full LV coverage, no gap; slice thickness 6 mm). For quantitative assessment of infarct morphology late gadolinium enhancement (LGE) was performed including measurement of total and relative infarct mass (related to LV mass) and the degree of transmurality (DT) as defined by the percentage of transmurality in each scar. (sequence parameters: inversion recovery gradient echo; matrix 256 × 148, imaging 10 min after 0.2 μg/kg gadolinium DTPA; slice orientation equal to SSFP). MRI images were analysed using dedicated software (MASS © , Medis, Netherlands). LGE was defined as myocardial areas with signal intensity above the average plus 5 SD of the remote myocardium. After implantation, patients were followed up including ICD readout after 3 and than every 6 months for a mean of 945 ± 344 days. ICD data were evaluated by an experienced electrophysiologist. Primary endpoint was the occurrence of an appropriate discharge (DC), antitachycard pacing (ATP) or death from cardiac cause. Results: The endpoint occurred in 10 patients (3 DC, 6 ATP, 1 death). These patients had a higher relative infarct mass (28 ± 7% vs. 22 ± 11%, p = 0.03) as well as high degree of transmurality (64 ± 22% vs. 44 ± 25%, p = 0.05). Their LVEF (29 ± 8% vs. 30 ± 4%, p = 0.75), LV mass (148 ± 29 g vs. 154 ± 42 g, p = 0.60), LVEDV (270 ± 133 ml vs. 275 ± 83 ml, p = 0.90) or total infarct mass (43 ± 19 g vs. 37 ± 21 g, p = 0.43) were however not significant from the group with no events. In a cox proportional hazards regression model including LVEF, LVEDV, LV mass, DT and age, only degree of transmurality and relative infarct mass emerged as independent predictors of the primary end point (p = 0.009). Conclusion: In CMI-patients fulfilling MADIT criteria ceCMR could show that the extent and transmurality of myocardial scarring are independent predictors for life threatening ventricular arrhythmia or death. This additional information could lead to more precise risk stratification and might reduce adverse events and cost of ICD therapy in this patient population. Larger trials are needed to confirm this finding.
European Heart Journal - Cardiovascular Imaging, 2013
Ventricular tachycardia (VT) is the commonest cause of sudden cardiac death (SCD) in developed countries. Coronary artery disease (CAD) is the most frequent cause of VT in individuals over the age of 30, while hypertrophic cardiomyopathy (HCM), myocarditis and congenital heart disease in those below 30 years of age. Cardiac magnetic resonance (CMR), a non-invasive, non-radiating technique, can reliably detect the changes in ventricular volumes and the ejection fraction that can be predictive of VT/SCD. Furthermore, the capability of CMR to perform tissue characterization and detect oedema, fat and fibrotic substrate, using late gadolinium enhanced images (LGE), can predict VT/SCD in both ischaemic and non-ischaemic cardiomyopathy. The extent of LGE in HCM is correlated with risk factors of SCD and the likelihood of inducible VT. In idiopathic-dilated cardiomyopathy, the presence of midwall fibrosis, assessed by CMR, also predicts SCD/VT. Additionally, in arrhythmogenic right ventricle (RV) dysplasia/cardiomyopathy, CMR has an excellent correlation with histopathology and predicted inducible VT on programmed electrical stimulation, suggesting a possible role in evaluation and diagnosis of these patients. A direct correlation between LGE and VT prediction has been identified only in chronic Chagas' heart disease, but not in viral myocarditis. In CAD, infarct size is the strongest predictor of VT inducibility. The peri-infarct zone may also play a role; however, further studies are needed for definite conclusions. Left ventricle, RV, right ventricular outflow tract (RVOT) function, pulmonary regurgitation and LGE around the infundibular patch and RV anterior wall play an important role in the VT prediction in repaired Tetralogy of Fallot. Finally, in treated transposition of great arteries, the extent of LGE in the systemic RV correlates with age, ventricular dysfunction, electrophysiological parameters and adverse clinical events, suggesting prognostic importance.
Related topics

Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
 Carlo Liguori
Carlo Liguori