Atlas of Flexible Bronchoscopy

Sign up for access to the world's latest research
Abstract
I would like to dedicate this book to my family for all their support and encouragement despite the endless evenings and weekends spent on this book. A special thanks to my wife, Mala who created some of the initial anatomical drawing for this book.

































































































































































































































































































































































![Fig. 8.8] Ultrasound image of the azygos vein at a lower level draining into the superior vena cava.](https://figures.academia-assets.com/41150239/figure_373.jpg)






















































































































































































































































Key takeaways
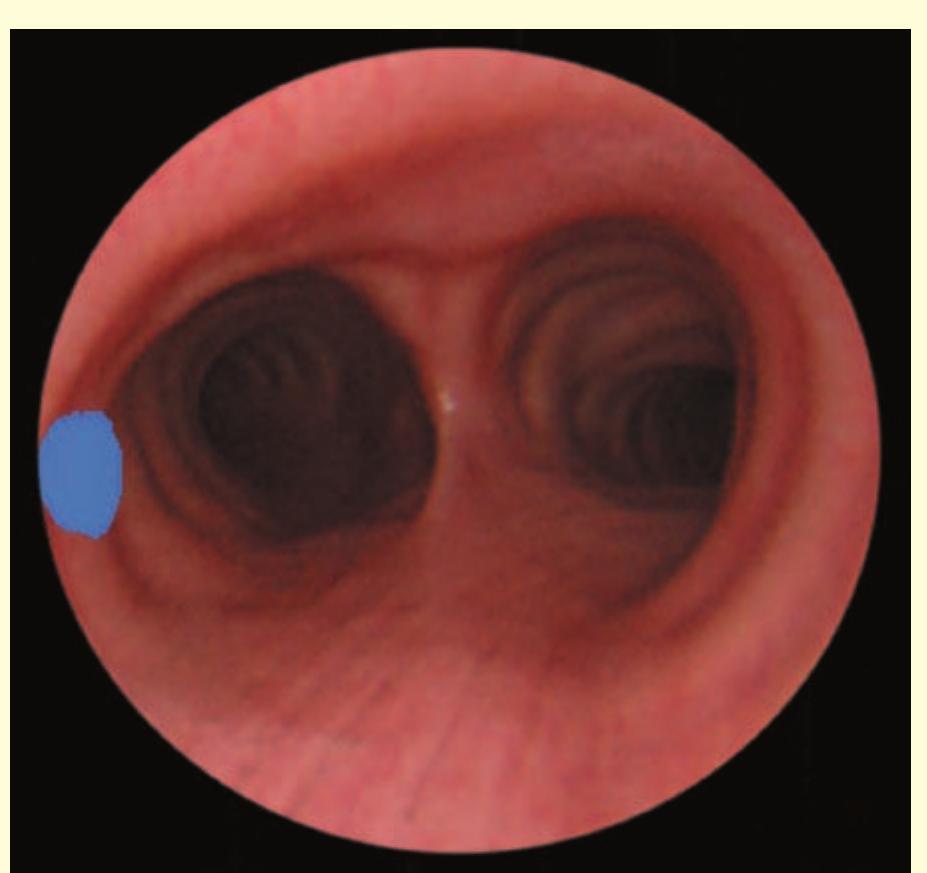
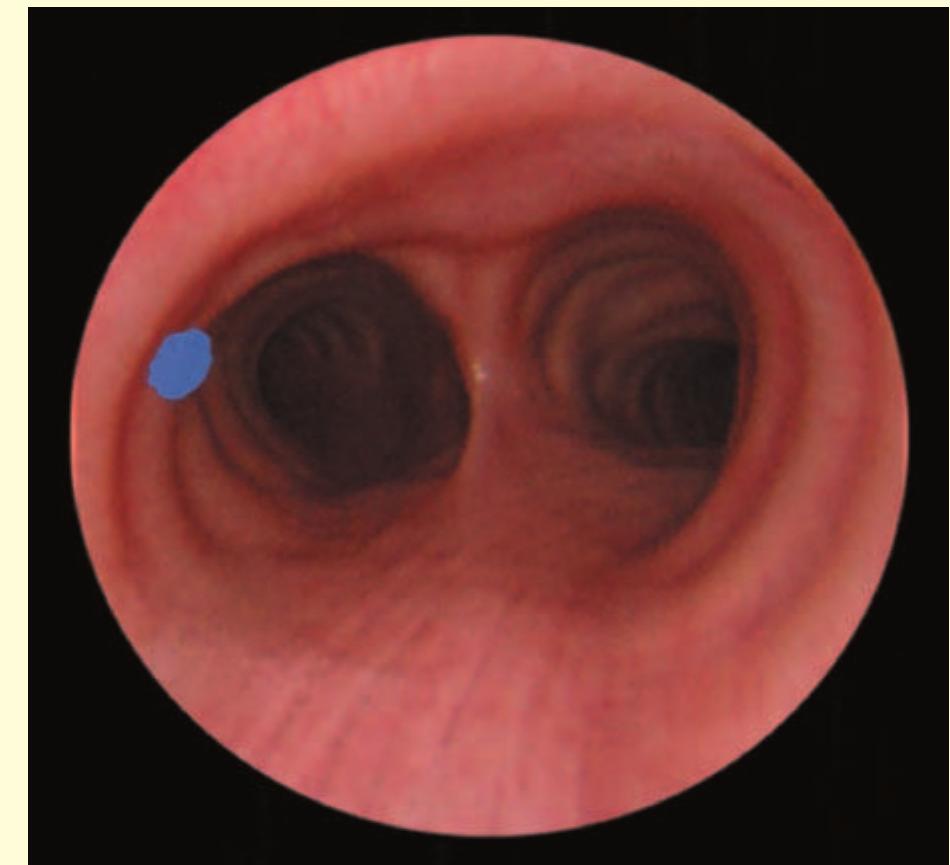
- The bronchoscope is then rotated anticlockwise by 150° to examine the subcarinal lymph nodes (station 7), extending down to the distal margin of the bronchus intermedius.
- Superior to the 11R lymph node, the right upper lobe bronchus and pulmonary artery may be visible.
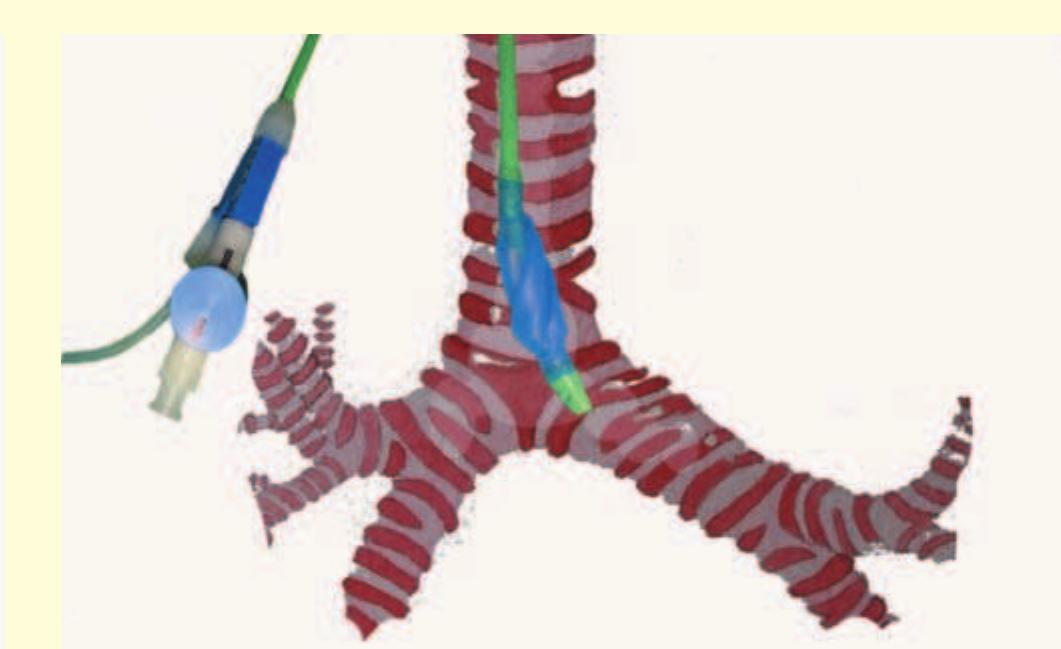
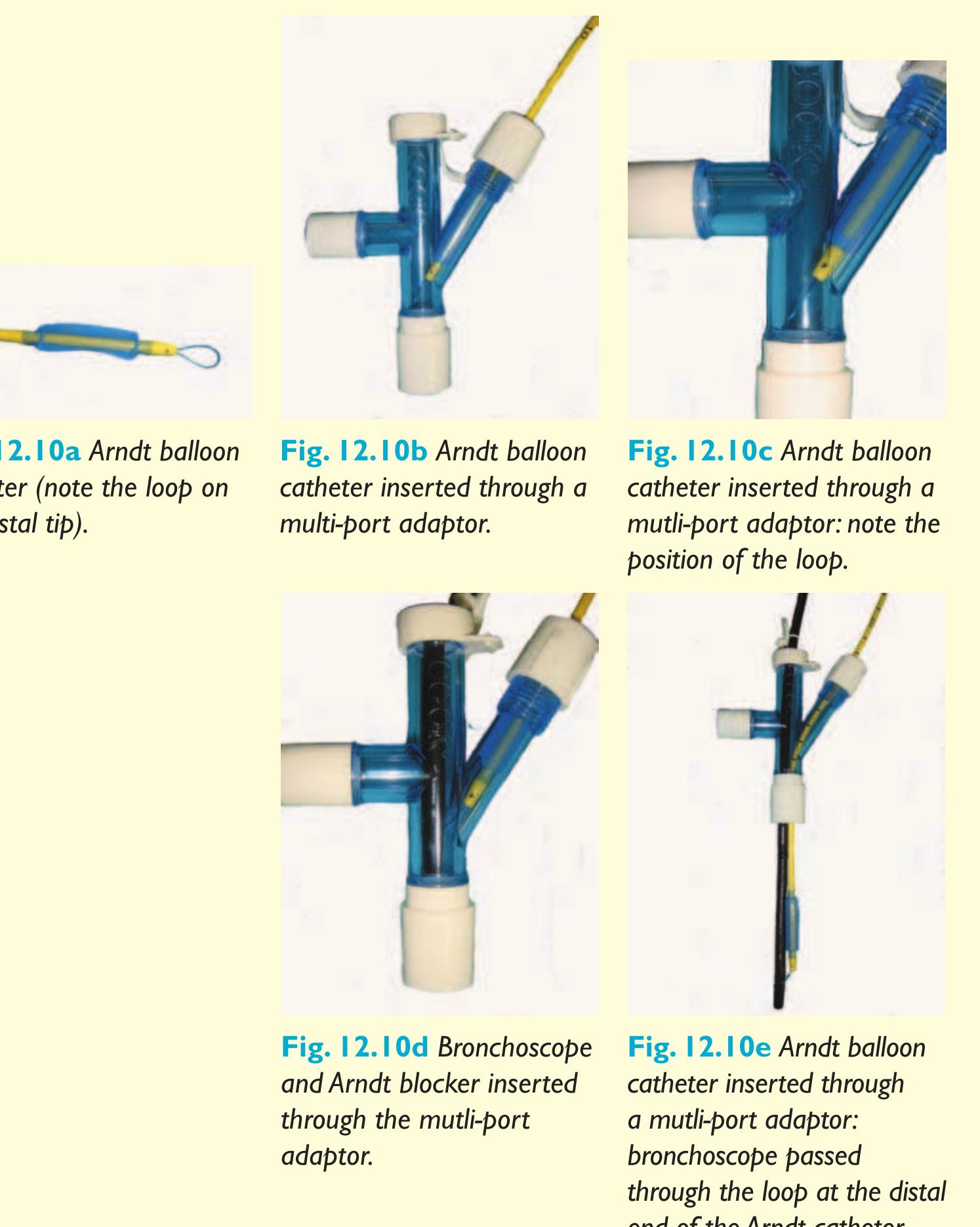
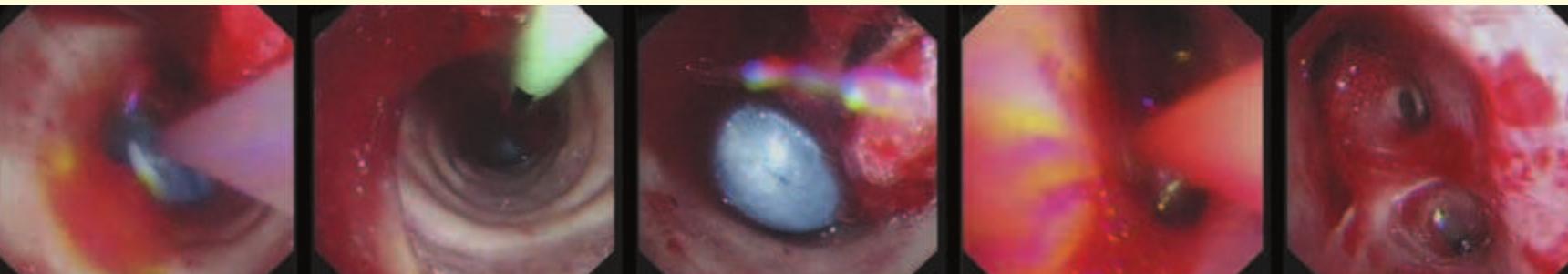
- Once the loop is tightened around the bronchoscope, the endobronchial blocker can be guided to any lobar bronchus (Fig. 12.11).
- Bronchoscopy with the nasal approach is performed and a polyethylene catheter is placed through the instrument channel of the bronchoscope and into the desired airway.
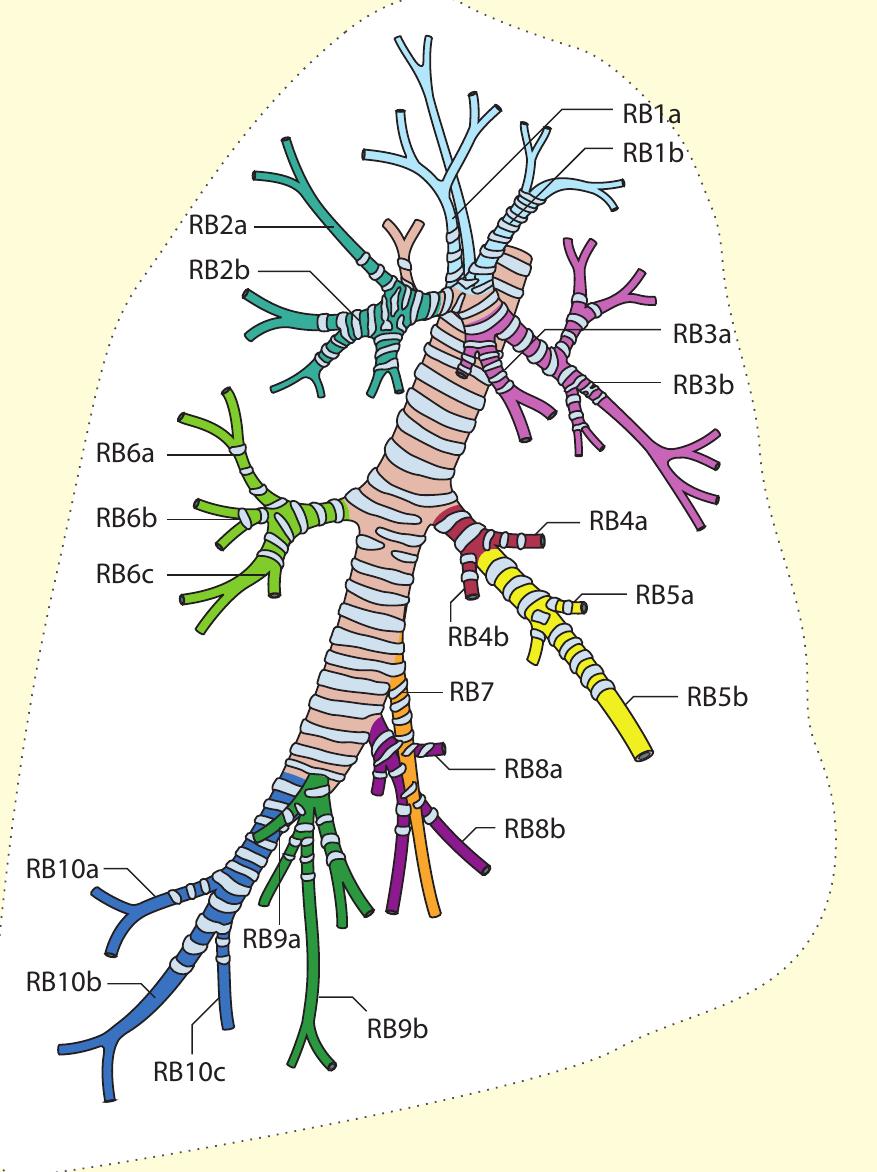
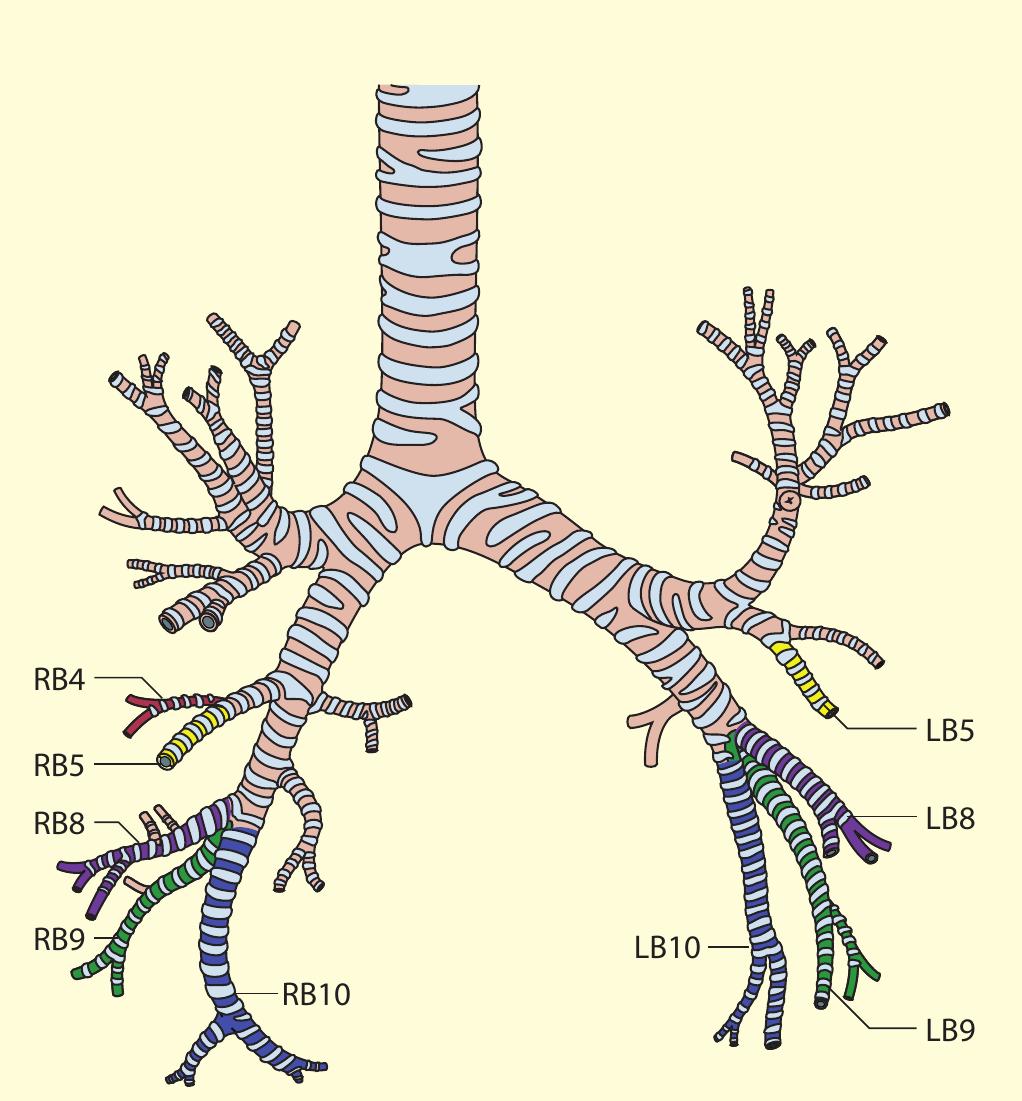
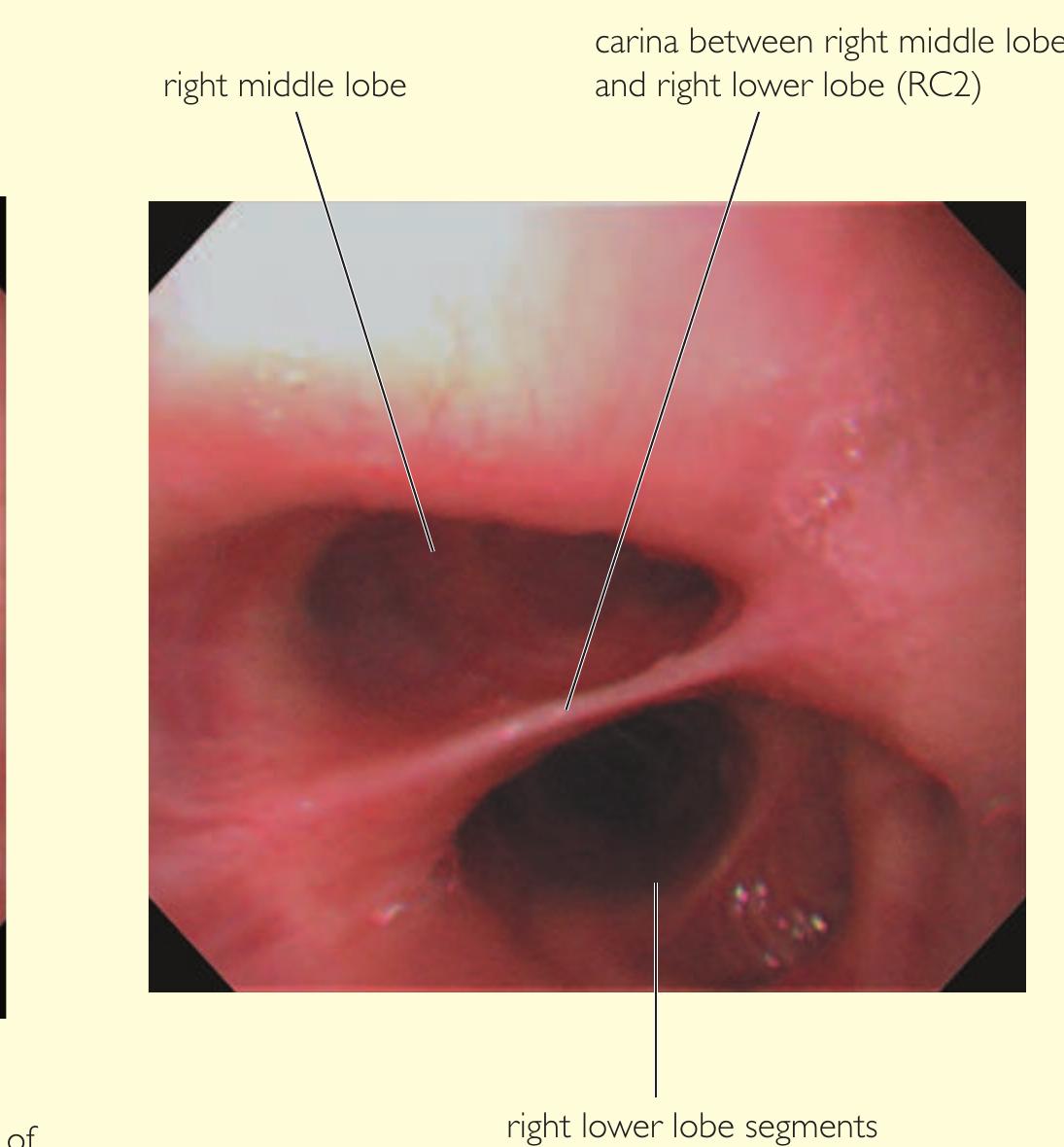
- Our approach, for example, for the right lower lobe is to treat RB10 (right posterior basal bronchus) first, using the BF260 bronchoscope (external diameter 4.3 mm) so that the distal subsegments can be assessed.
Related papers
The Indian Journal of Pediatrics, 2015
Bronchoscopes have markedly improved the diagnosis as well as therapy in pediatric pulmonary disorders. Two types of bronchoscopes are available; flexible and rigid, with their own advantages and disadvantages. Depending on the clinical need and availability of skills, choice is made between the two. Typically, rigid scopes are largely used by the surgeons (pediatric or otolayngologists) while flexible bronchoscope stays in the domain of the pediatric pulmonologist and intensivists. Rigid scopes may be more versatile than flexible bronchoscopes in removing the foreign bodies from the airway. Flexible bronchoscopes on the other hand can even be introduced through an endotracheal tube. At times, use of both scopes may be required in a given patient for optimal results. Bronchoscopes give us a means to visualize the inside of the airway, which can be very informative for assessing various pathologies affecting the airways. Apart from the visualization of the parts of the airway tree and their structure as well as patency, it can also be used to take tissue biopsy specimens, collect secretions from the airways and bronchoalveolar lavage which can also get cellular elements from the distal alveoli. In the past few decades, more and more instruments are being used for expanding the utility of flexible bronchoscope for interventions ranging from bronchial toilet, foreign body removal, airway stenting and lasers or cryotherapy for airway lesions. The perinatologists have opened up more vistas and thrown newer challenges for using fiberoptic bronchoscopy (FB) for in utero tracheal occlusion in cases with diaphragmatic hernia. The vast applications of this tool makes it very relevant to pulmonary investigations and therapeutics.
Medicine, 2008
Bronchoscopy is an essential tool in respiratory medicine, which allows visualization and sampling from the main airways. It has an important role in the evaluation of suspected lung cancer, interstitial lung disease, persistent infection and the assessment of new pulmonary infiltrates in immunocompromised patients. It is a very safe technique which can be performed with or without conscious sedation. Recent developments have ranged from the improvement in image quality to integration of ultrasound. this has increased diagnostic sensitivity and facilitated imageguided biopsies of masses beyond the airways. the therapeutic role of bronchoscopy is also expanding from lung cancer to airways disease.
Lung India, 2015
deployment of metallic stents and others) procedures. FB is an easy to perform and a safe procedure. [2,3] Unlike its rigid counterpart, FB can be performed under conscious sedation and local anesthesia thereby avoiding the attendant complications of general anesthesia. Moreover, FB is an outpatient procedure, thus obviating the need for hospitalization. Furthermore, FB can be used to observe upper lobes and bronchial subsegments that are not easily visualized by a rigid bronchoscope. [4-9] FB is now widely performed in India and is considered an essential requirement for a pulmonologist. Herein, we describe our experience of performing FB over the last three-and-a-half decades.
Einstein (São Paulo)
Objective: To describe indications, clinical outcomes and complications of flexible bronchoscopy. Methods: A descriptive observational study of bronchoscopies performed at the endoscopy service of Hospital Israelita Albert Einstein. Demographic (age, gender and origin) and medical (indications and results of endoscopy and diagnostic tests, such as biopsy collection, lavage, cytology and culture) data were analyzed. Electronic medical records with incomplete data or reporting interventional procedures were excluded. Results: Over a three-year period (2013 to 2016), a total of 1,949 bronchoscopies were performed by respiratory endoscopy team and anesthesia specialists of the hospital. The mean age of patients was 57.7±21.9 years (range of 3 days to 99 years), with prevalence of males (56.4%). The procedures were mostly (86.3%) elective and 30.7% were carried out in the intensive care unit. Major indications for bronchoscopy were infection or secretion (42.4%), followed by suspected neoplasm (10.8%). Endoscopic changes were reported in 91.9% of cases, with more than one change described in approximately 6.9% of patients. Positive results were obtained via direct testing or culture in 36.3% and 53.9% of 1,399 bronchoalveolar lavages, respectively. The overall diagnostic yield (bronchoalveolar lavage and biopsy) was 72.6%. Mild adverse event rate was 7.2%. The rate of severe adverse events requiring additional intervention was 0.5% (pneumothorax, 0.4%; severe bleeding with patient death, 0.1%). Conclusion: Lower airway endoscopy is critical for respiratory disease assessment, diagnosis and treatment. Flexible bronchoscopy is associated with good diagnostic yield and minimal inherent risk.
Clinics in Chest Medicine, 2013
Interventional pulmonology Interventional bronchoscopy Rigid bronchoscopy Flexible bronchoscopy Airway stenting Airway obstruction Airway stenosis
Global Perspectives on Bronchoscopy, 2012
A recent trend has been the emergence of "interventional bronchoscopy" and the "interventional bronchoscopist". These phrases denote a two-tier system in which one group of bronchoscopists perform "routine bronchoscopy" and the other performs special bronchoscopic procedures. Disease processes encompassed within this discipline include complex airway management problems, benign and malignant central airway obstruction, pleural diseases, and pulmonary vascular procedures. Diagnostic and therapeutic procedures pertaining to these areas include, but are not limited to, rigid bronchoscopy, transbronchial needle aspiration (TBNA), auto fluorescence bronchoscopy, endobronchial ultrasound (EBUS), transthoracic needle aspiration (TTNA) and biopsy, laser bronchoscopy, endobronchial electrosurgery, argon-plasma coagulation, cryotherapy, airway stent insertion, balloon bronchoplasty and dilatation techniques, endobronchial radiation, photodynamic therapy, percutaneous dilatational tracheotomy, transtracheal oxygen catheter insertion, medical thoracoscopy, and imaging-guided thoracic interventions. (Anders et al. 1988) Considering the prominence of FFB in the procedural armamentarium of pulmonary physicians (among other specialties) and the new developments of interventional bronchoscopy, it is important for the non-interventional pulmonologist and physician in pulmonary training to have a clear understanding of the role of FFB.
Ghana Medical Journal, 2021
Objectives: Flexible Fibreoptic bronchoscopy (FFB) is a major diagnostic and therapeutic tool employed largely in respiratory medicine but its use in our country has been quite limited. We performed a retrospective review of the indications, overall diagnostic yield and safety of FFB at the Korle-Bu Teaching Hospital (KBTH).Study Design: Retrospective studyStudy Setting: Cardiothoracic Unit, Korle-Bu Teaching HospitalStudy Participants: All bronchoscopy records from January 2017 - December 2018Interventions: Eight-five bronchoscopy reports generated over a 2-year period were reviewed. Using a data extraction form, patient’s demographic details, indications for FFB, sedation given, specimen obtained and results of investigation, and complications encountered were recorded and entered into SPSS version 22. Descriptive analysiswas performed and presented as means and percentages.Results: Suspected lung cancer was the predominant indication for bronchoscopy requests (55.3%). Diagnostic ...
Journal of Thoracic Disease
German laryngologist Gustav Killian performed the first "Direkte Bronchoskopie" using a rigid bronchoscope to extract a foreign airway body from the right main bronchus over a hundred years ago, transforming the practice of respiratory medicine. The procedure instantaneously became popular throughout the world. Chevalier Jackson Sr from the United States further advanced the instrument, technique, safety, and application. In the 1960s, Professors Harold H. Hopkins and N.S. Kapany introduced optical rods as well as fiberoptics that led Karl Storz to develop the cold light system improving endoluminal illumination, achievements that ushered in the modern era of flexible endoscopy. Several diagnostic and therapeutic procedures became possible such as transbronchial needle biopsy, transbronchial lung biopsy, airway electrosurgery, or cryotherapy. Dr. Jean-François Dumon from France advanced the use of Nd-YAG laser in the endobronchial tree and created the dedicated Dumon silicone stent introducing the whole new field of interventional pulmonology (IP). This major milestone revitalized interest in rigid bronchoscopy (RB). Now, advancements are being made in stenting, instrumentation, and education. RB robotic technology advancements are currently anticipated and can potentially revolutionize the practice of pulmonary medicine. In this review, we describe some of the most substantial advances related to RB from its beginning to the modern era.
Panminerva Medica, 2019
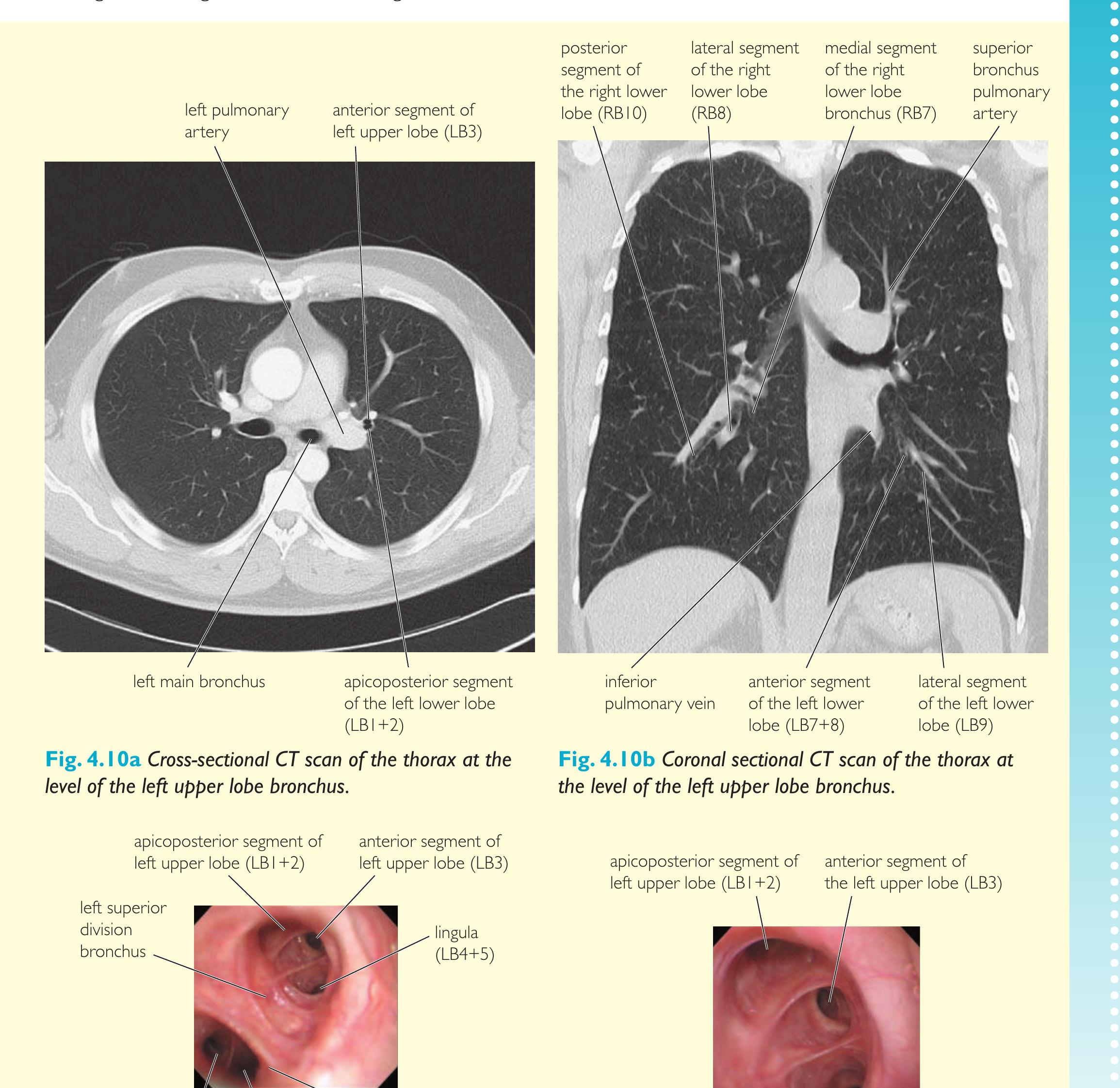
Diagnostic bronchoscopy and tissue sampling techniques using forceps (endobronchial biopsy [EBB] and transbronchial biopsies [TBB]) or needle aspiration (transbronchial needle aspiration-TBNA), all performed with a flexible bronchoscope, are the basic elements of any interventional procedure. The flexible fibrobronchoscopy allows the visualization of the airways and is used both for diagnostic and therapeutic purposes. The working channel of both fibrobronchoscopes with optical fibers and videobronchoscopes, even if of relatively small diameter, allows the insertion of various diagnostic and therapeutic accessories. Fiber optic systems have been widely replaced by video cameras using a miniaturized charge-coupled device camera positioned at the end of the scope that provides electronic transmission of images to a monitor. The indications for both diagnostic and therapeutic fibrobronchoscopy derive from a correct evaluation of symptoms and objective signs of the patient and from the correct interpretation of imaging methods. Although bronchoscopy techniques keep evolving at a rapid pace, basic procedures such as bronchoalveolar lavage, transbronchial lung biopsy, and transbronchial needle aspiration still play a key role in pulmonary disease diagnostics, and therefore, these methods must still be part of the training of interventional pulmonologists. Trainees will acquire a thorough knowledge of thoracic anatomy and become skilled in the interpretation of thoracic imaging, after which they will be given a theoretical and practical training course on virtual reality simulators, on animal or cadaver models, the effectiveness of which has been fully demonstrated by scientific studies. Specific DOPS tests have been developed for a qualitative evaluation of procedures on simulators, on animal models and on the patient.
Lung Cancer Management, 2017
During routine endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) procedures, especially with biopsy of lymph nodes in or around the left upper lobe, frequent reports have noted the loss of ultrasound image and needle angulation leading to an inability to biopsy nodes visualised by EBUS. The aim of this research was to investigate and compare this loss of angulation with commercially available scopes. Bench-top experiments and a clinical case study demonstrated the varying loss of scope angulation, flexibility and manoeuvrability with different scopes and biopsy instruments leading to procedural implications. Improvements in both the EBUS scope and needle characteristics are required to overcome this limitation which has implications in bronchoscope navigation and the diagnostic yield of EBUS-TBNA.
Background and objectives: The flexible bronchoscope has become widely used by pediatric pulmonologists as a diagnostic and therapeutic tool. Nevertheless, there are several gaps in our knowledge to help refine its use and reduce its complications. In this study, we aimed to evaluate the utility and complications of pediatric bronchoscopy. Design and setting: We conducted a retrospective review of bronchoscopy cases between March 2006 and April 2015 at a tertiary care medical center (King Fahad Medical City). One-hundred forty nine patients were studied. Patients and methods: We evaluated how bronchoscopy contributed to the patients' diagnosis, assessed the accuracy of bronchoalveolar lavage white blood cell count (BAL WBC) to differentiate between infectious and non-infectious conditions, assessed the ability of clinical factors to predict high risk of desaturation during bronchoscopy, and finally summarized the reported procedural complications. Results: We found pediatric bronchoscopy was a crucial diagnostic (confirming, ruling out, and discovering unexpected diagnosis) and therapeutic tool. The accuracy of BAL WBC counts is poor (AUC (95% CI) Z 0.609 (0.497e0.712)); however, using two cutoff values (10 WBCs (sensitivity Z 84.44% and specific ity Z 2 9.27%) to rule out, and !400 WBCs (sensitivity Z 33.33% and specificity 81.49%) to rule in infection) helped in early differentiation between infectious and non-infectious conditions. From the factors that we test, none we found predictive of desaturation. The most common procedural complication was International Journal of Pediatrics and Adolescent Medicine (2016) 3, 18e27 desaturation (pooled incidence (95% CI) Z 13 (8e19)%) followed by cough, mild airway bleeding, and spasm. Conclusions: Flexible bronchoscopy is an important and relatively safe diagnostic and therapeutic tool in pediatric medicine, and utilization of this service should be encouraged after a careful consideration of which patient needs this procedure and a rigorous estimate of its pros and cons.
2020
A 12-year-old girl presented with chronic suppurative lung disease secondary to an old forgotten, foreign body (plastic whistle) in the right lower lobe bronchus, confirmed by Contrast enhanced computer tomography (CECT) chest. Rigid bronchoscopic removal was attempted twice but the foreign body could not be removed. Under general anesthesia, a flexible bronchoscope was inserted through the rigid bronchoscope and the foreign body was grasped and removed using rat-toothed forceps inserted through the suction channel of the flexible scope. Although there are a few reports of sequential use of flexible and rigid bronchoscopies, this report highlights the feasibility and utility of flexible through rigid bronchoscopy technique for foreign body removal in the distal airways.
Clinics in Chest Medicine, 2010
The Medical journal of Malaysia, 2003
All children who underwent flexible bronchoscopy in the respiratory unit at Paediatric Institute, Hospital Kuala Lumpur from June 1997 to June 2002 were reviewed. A hundred and ten children underwent the procedure under sedation or general anaesthesia. The median age of these children was eight months. (Q1 3, Q3 30) The commonest indication for performing flexible bronchoscopy was for chronic stridor (50 cases) followed by persistent or recurrent changes such as lung infiltrates, atelectasis and consolidation on the chest radiographs (22). Laryngomalacia was found to be the commonest cause of stridor in 29 children. Two patients were diagnosed with pulmonary tuberculosis. With regard to safety, three procedures were abandoned due to recurrent desaturation below 85%. One of these patients had severe laryngospasm that required ventilation for 48 hours but recovered fully. Two neonates developed pneumonia requiring antibiotics following bronchoscopy. No patients developed pneumothorax ...
Saudi medical journal
lexible fiber optic bronchoscopy (FFB) was introduced by S. Ikeda in 1964. Since then bronchoscopy has become an important diagnostic and therapeutic tool for management of chest disease. The indications of bronchoscopy are numerous and usually based on the presence of respiratory symptoms and abnormal chest radiograph or both. 1 Common indications include peripheral pulmonary nodule, hemoptysis, chronic cough, pleural effusion, recent or unresolved pneumonia, pulmonary tuberculosis, and lung collapse. 2-9 Bronchoscopy can be used in the intensive care units as an aid for intubation, positioning of double lumen tubes for surgery, and in the diagnosis of ventilation-Objectives: To review the safety, indications, complications of flexible fiberoptic bronchoscopies performed at university teaching hospital, and to correlate the bronchoscopic findings with radiology, histology, and history of smoking.
Interactive CardioVascular and Thoracic Surgery, 2007
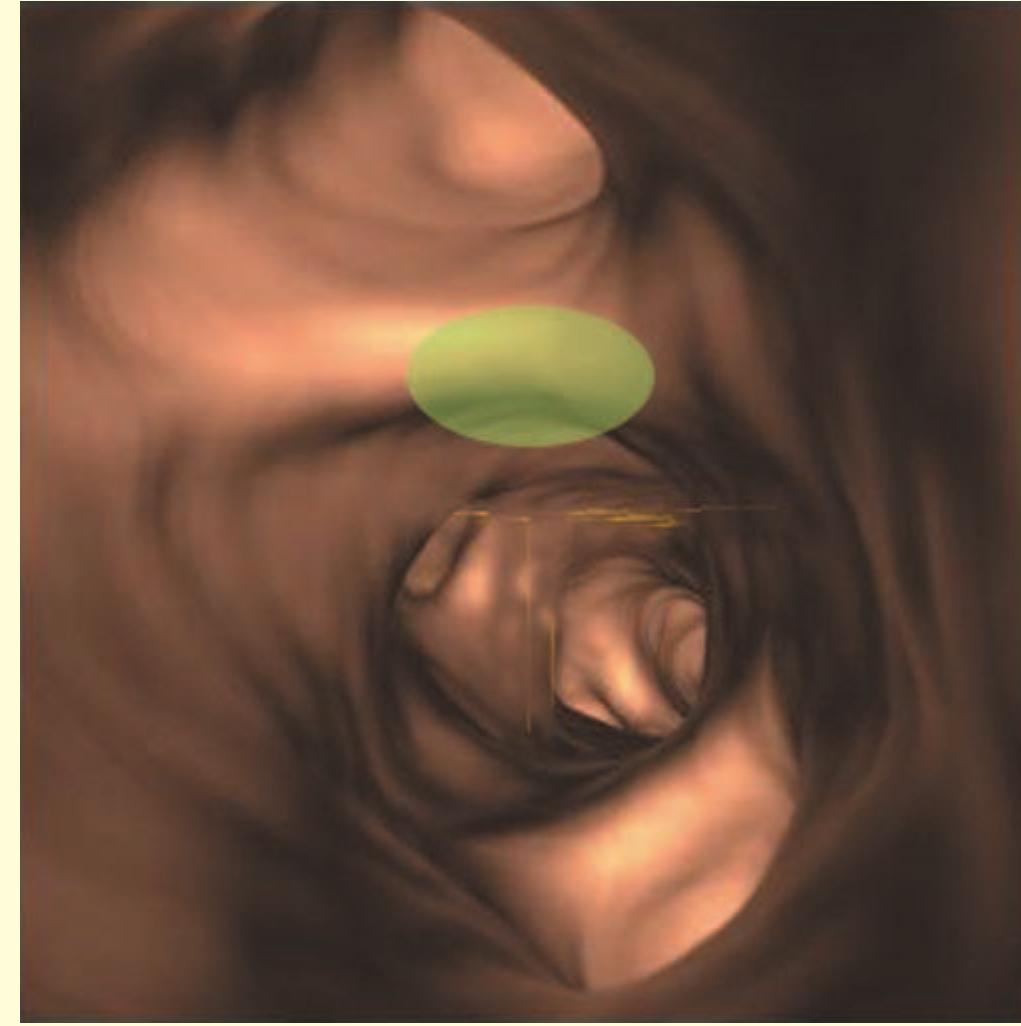
Flexible fiberoptic bronchoscopy is an indispensable tool for optimal management of intensive care unit patients. However, the acquisition of sufficient training in bronchoscopy is not straightforward during residency, because of technical and ethical problems. Moreover, the use of commercial simulators is limited by their high cost. In order to overcome these limitations, we realized a low-cost anatomical simulator to acquire and maintain the basic skill to perform bronchoscopy in ventilated patients. We used 1.5 mm diameter iron wire to construct the bronchial tree scaffold; glazier-putty was applied to create the anatomical model. The model was covered by several layers of newspaper strips previously immersed in water and vinilic glue. When the model completely dried up, it was detached from the scaffold by cutting it into six pieces, it was reassembled, painted and fitted with an endotracheal tube. We used very cheap material and the final cost was 716. The trainer resulted in real-scale and anatomically accurate, with appropriate correspondence on endoscopic view between model and patients. All bronchial segments can be explored and easily identified by endoscopic and external vision. This cheap simulator is a valuable tool for practicing, particularly in a hospital with limited resources for medical training.
Critical Care Nurse, 2011
endotracheal intubation in order to ensure airway patency and minimize risks of procedure-related respiratory insufficiency. 4-7 In many instances, however, bronchoscopy can be safely performed while the patient receives NPPV, sparing patients the discomfort and risks of refractory hypoxemia, intubation, and mechanical ventilation. The limited available published evidence indicates that NPPVassisted flexible bronchoscopy is used about 3 times per month in tertiary academic centers. Critical care nurses have an essential role in the preparation and performance of this procedure, as well as in surveillance after the procedure, and, as part of the multidisciplinary health care team, in patient care decisions. The objectives of this article, therefore, are to review the physiological basis for NPPV-assisted bronchoscopy; describe its indications, contraindications, and techniques; and identify ways in which critical care nurses can further influence patient care before, during, and after this airway procedure.
Multimedia Manual of Cardiothoracic Surgery
Palliative airway treatments are essential to improve quality and length of life in lung cancer patients with central airway obstruction. Rigid bronchoscopy has proved to be an excellent tool to provide airway access and control in this cohort of patients. The main indication for rigid bronchoscopy in adult bronchology remains central airway obstruction due to neoplastic or non-neoplastic disease. We routinely use negative pressure ventilation (NPV) under general anaesthesia to prevent intraoperative apnoea and respiratory acidosis. This procedure allows opioid sparing, a shorter recovery time and avoids manually assisted ventilation, thereby reducing the amount of oxygen needed, while maintaining optimal surgical conditions. The major indication for NPV rigid bronchoscopy at our institution has been airway obstruction by neoplastic tracheobronchial tissue, mainly treated by laser-assisted mechanical dissection. When strictly necessary, we use silicone stents for neoplastic or cicat...
endotracheal intubation in order to ensure airway patency and minimize risks of procedure-related respiratory insufficiency. 4-7 In many instances, however, bronchoscopy can be safely performed while the patient receives NPPV, sparing patients the discomfort and risks of refractory hypoxemia, intubation, and mechanical ventilation. The limited available published evidence indicates that NPPVassisted flexible bronchoscopy is used about 3 times per month in tertiary academic centers. Critical care nurses have an essential role in the preparation and performance of this procedure, as well as in surveillance after the procedure, and, as part of the multidisciplinary health care team, in patient care decisions. The objectives of this article, therefore, are to review the physiological basis for NPPV-assisted bronchoscopy; describe its indications, contraindications, and techniques; and identify ways in which critical care nurses can further influence patient care before, during, and after this airway procedure.
Pediatric Pulmonology, 2017
Aim: Eighteen years have passed since the last European survey concerning practices in pediatric bronchoscopy was conducted. Therefore, members of the European Respiratory Society (ERS) Pediatric Bronchology Group 7.7, initiated the "European Pediatric Bronchoscopy Survey 2015," which aimed to assess the current state of this evolving diagnostic and therapeutic procedure in the field of pediatric respiratory medicine. Method: A questionnaire was sent to national representatives of 44 European countries with the request to distribute it to all centers performing pediatric bronchoscopies. Questions concerned the following areas of interest: number of procedures, personnel and technical equipment, indications, complications, anesthesia, and diagnostic possibilities. Results: In total, 198 European centers from 33 European countries participated in the survey. From 2012 to 2014 a total of 57 145 bronchoscopies were reported. Both flexible and rigid techniques were available at most of the centers. The most frequently mentioned indications were suspected aspiration, infection, radiographic abnormalities, airway obstruction, and cough. Hypoxemia, airway obstruction, and cough were the most common complications mentioned, followed by airway hemorrhage. Most centers were able to perform bronchoalveolar lavage (BAL) and endobronchial biopsies and some performed more special procedures, such as transbronchial biopsies. Interventions like balloon dilation, laser procedures, or stent placement were less common and rarely available. Conclusion: Compared to the 1997 survey, our results suggest that pediatric bronchoscopy has become more widely available and established in Europe. Different practices in individual countries suggest that more effort should be put on standardizing bronchoscopic procedures across Europe.
Related topics

Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
 Johnny Pujols
Johnny Pujols